News
Pet of the month – August – Max
by admin on August 1st, 2018
Category: Pet of the Month, Tags:
Max is recovering from a severe anaemia caused by a flea infestation. The severity was in fact so great that Max had to have an emergency blood transfusion, and his coat was completely shaved off.
Fleas are a blood sucking parasite and in sufficient numbers can deplete the number of red blood cells circulating in the body. The very prolonged warm spell we are having is causing flea numbers to rise exponentially. Each flea can lay up to 50 eggs daily and these can hatch within 14 days in hot weather. Although it is extremely unusual for a pet to be parasitised by fleas to this extent it is a warning to us all to maintain flea and all anti-parasite control this summer.
Pododermatitis
by admin on August 1st, 2018
Category: News, Tags:
What is pododermatitis?
Pododermatitis is a term used to describe inflammation affecting the skin of the feet. It often causes dogs to have swollen, red and itchy feet, which can progress to painful sores if left untreated. In very severe cases, dogs can even become lame. This is a relatively common skin problem in dogs and can be present on its own or as part of a more widespread skin problem. There are many causes of pododermatitis and in some patients more than one cause is present at the same time. It is important to obtain an accurate diagnosis so that the right treatment can be selected.
What causes pododermatitis?
Parasites
The parasitic mite Demodex can infect the haired skin of the feet and result in pododermatitis. Demodex mites are present in very low numbers in the skin of all dogs, but in some patients, either due to a genetic susceptibility, or due to a process that lowers the immune system, these mites can populate the skin in very large numbers causing disease. Pododermatitis due to these mites tends to result in hair loss, swelling and bleeding sores in some cases. This mite is not infectious to other animals or people, but requires specific treatment to reduce mite numbers down to normal levels again. Very rarely, other parasites can also contribute to pododermatitis.
Foreign bodies
Foreign bodies like grass seeds are a very common cause of pododermatitis in dogs. Foreign bodies tend to penetrate the skin of the feet when dogs are out walking/running and then trigger inflammation when they become trapped within the feet. The body often attempts to ‘expel’ these structures resulting in painful and often discharging lumps between the toes. Affected patients often lick and chew at the affected sites. Foreign bodies are particularly likely when one lesion is present on one foot.
Allergies
Allergic diseases in dogs and cats are very common, and results in inflammation in the skin. This inflammation is very commonly seen affecting the feet, and results in redness, excessive licking and chewing at the affected sites. The most common triggers for allergic pododermatitis are food items and environmental substances such as dust mites and pollens, and skin disease usually starts in early life between the ages of 6 months and 3 years.
Deep infections
A very common feature of pododermatitis, particularly in dogs, is a deep infection of the feet. This is usually due to bacteria, but can be due to rare fungal organisms, and often results in multiple painful, swollen and discharging lumps. Affected animals usually lick and chew excessively and can become lame in severe cases. Bleeding lesions are relatively common with deep infections.
Conformation
A frustrating cause of pododermatitis is termed conformational pododermatitis. This usually occurs in heavy set dogs with excessively splayed feet. This results in weight bearing on hairy parts of the foot adjacent to the footpads and triggers inflammation of the hair follicles. Over time, this inflammation damages the hair follicles and results in chronic inflammation with the feet. Dogs with this condition tend to have large areas of pad extension, with painful and swollen lumps around the toes.
Hormonal diseases
Certain hormonal diseases can also be involved in the development of pododermatitis as the local skin immune system is reduced and the ability to fend off infections is compromised. The most commonly involved diseases include an underactive thyroid gland (hypothyroidism) or overactive adrenal glands (Cushing’s disease). However, pododermatitis is a relatively rare symptom of these diseases and dogs and cats usually show other more characteristic symptoms.
How is pododermatitis diagnosed?
Diagnosis of pododermatitis can often be achieved following a thorough evaluation of the history and clinical signs. Hair plucks and skin scrapings are performed to diagnose Demodex mite infestation and swab samples are often taken to establish if an infection is present. If lumps are discharging fluid, a sample of this fluid may also be sent to a laboratory to grow (culture) any infectious organisms. If the clinical picture is very suggestive of a foreign body, X-rays may be needed along with a surgical procedure to remove the offending item. Allergies are often only diagnosed once infections/parasites are treated and removed. If redness and inflammation remain, allergy testing may be required. Hormonal diseases are often suspected if other clinical signs are present but usually require blood testing to diagnose. Conformational pododermatitis is usually diagnosed by examining the feet and assessing the shape (conformation) of the footpads.
What are the treatments available?
Treatments for pododermatitis vary depending on the underlying cause. Parasitic infestations are usually treated with dips/rinses for the feet. Deep infections are often treated with long courses of antibiotics or antifungal medications in the rare cases due to fungal infection. Foreign bodies are best treated by identifying the foreign body and removing it in a minor surgical procedure. Hormonal diseases require treatment specific to the condition, but sometimes involve supplementing with hormone, as is the case in hypothyroidism. Allergic diseases are treated by identifying the triggers and removing them if possible.
Conformational pododermatitis is perhaps the most difficult to treat, as the defect is due to the conformation of the patient. Many of these cases can only be managed rather than cured and require modifications such as protective boots, good foot hygiene and avoidance of rough and uneven terrain. In some of the very worst cases, conformational pododermatitis can be corrected with surgery to fuse the toe webs together.
What is the prognosis?
As there are numerous causes of pododermatitis and more than one can be present at the same time, a good prognosis depends on identifying all the contributing factors and correcting them if possible. If this can be done, the vast majority of cases will have a good outcome. Cases of conformational pododermatitis are rarely cured, and require long term management.
Recurrent Corneal Ulcers (Indolent Ulcers)
by Hannah Wright on July 9th, 2018
Category: News, Tags:
What is the cornea?
The cornea is the clear window of the eye. It is a delicate structure which is less than a millimetre thick. In order to be transparent, the cornea has no blood vessels. It consists of three layers which are arranged like those of a sandwich. The three layers comprise: 1) the epithelium – this is the thin outer ‘skin’ of the cornea; 2) the stroma which is the much thicker middle layer of the ‘sandwich’; 3) the endothelium – this is the inner layer of the cornea and is very thin indeed (only one cell thick).
What is a corneal ulcer?
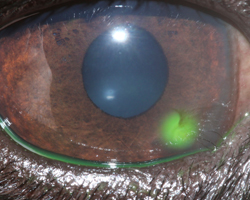
Any injury involving the cornea can be described as an ulcer. Generally, corneal ulcers are described as superficial or deep, depending on whether they just involve the outer skin (the epithelium), in which case they are called superficial ulcers or erosions – or whether they extend into the middle layer (the stroma), in which case they are called deep ulcers. The attached image shows the use of a dye called fluorescein which will stain ulcers and show up the defect. Most superficial ulcers heal rapidly as the cells of the surrounding outer ‘skin’ (the epithelium) slide and grow into the defect. The new skin that grows then sticks to the tissue underneath. Most superficial ulcers will have healed within a week.
How do I notice that my dog has an ulcer?
The cornea is sensitive because it has a lot of nerve endings, and ulceration is usually associated with quite marked discomfort because the nerves are exposed. Signs of eye discomfort include weeping, blinking, squinting, pawing at the eye and general depression.
What makes an ulcer indolent?
An indolent ulcer is an ulcer which fails to heal in the expected time. It then tends to cause ongoing discomfort and irritation. Eyes affected with indolent ulcers try to grow a new surface skin over the defect, but the incoming cells fail to stick down onto the layer underneath (the stroma). As a result, a thin layer of loose tissue can often be seen surrounding the ulcerated area. The reason why the cells fail to stick is not fully understood but is believed to be mainly because the epithelial cells fail to form tiny ‘feet’ that normally hold on to the tissue underneath.
Are certain breeds predisposed to develop indolent ulcers?
Certain breeds are predisposed to develop indolent ulcers – Boxers, Corgis, Staffordshire Bull Terriers and West Highland White Terriers are often affected. However, any dog can develop an indolent ulcer, and older patients are more commonly affected. Once a dog has suffered an indolent ulcer in one eye, it may develop one in the other eye, or recurrence of ulceration in the first eye. This can happen at any time after the first ulcer (sometimes years later).
What treatment options are available if my dog has an indolent ulcer?
It is not possible to achieve healing of indolent ulcers with the use of antibiotic or false tear ointments alone. In order for healing to occur, it is important that all loose tissue is removed and that the exposed stroma is treated and ‘freshened up’ to allow adhesion of new epithelial (‘skin’) cells. The process of removal of loose epithelium is called ‘debridement’ and in most patients it can be carried out with the use of local anaesthetic drops in the eye. Diamond Burr Debridement is the gold standard although other methods may be employed. Following the debridement, the exposed stroma is sometimes abraided with small dot-like scratches using a fine needle to allow the ‘feet’ of the new cells to take hold. The latter procedure is called a ‘punctate’ or ‘grid’ ‘keratotomy’.
In very fractious patients, it may be necessary to give a sedative to perform these procedures. More severe and longstanding cases require more radical treatment under a general anaesthetic. In this instance all diseased epithelium and some of the underlying stroma is removed. This procedure is carried out under the operating microscope with a sharp knife. The operation has a high success rate but is not suitable for every case.
What care will be required following debridement and cautery?
Usually, a broad spectrum antibiotic will be dispensed to be applied three times daily to help to prevent infection. In some cases, it may be necessary to give a drug (atropine) which widens the pupil and reduces pain associated with the ulcer. Often patients with an indolent ulcer will receive a painkiller which is given with food. In some patients, the pain associated with the ulcer appears more severe than in others.
How does the eye appear during healing of the ulcer?
In some patients, healing of the ulcer occurs fast and the cornea will only be slightly cloudy during treatment. However, in patients where healing of the ulcer is slow, it is common to find that blood vessels grow into the cornea and that pink granulation tissue forms to cover the defect. During this time, the eye may appear very red and odd looking. However, once the defect is fully covered, the granulation tissue will gradually clear over a period of months, leaving only minor corneal scarring in the majority of cases. Vision in most patients will return to normal or near normal after an episode of indolent ulceration.
How long does an indolent ulcer take to heal on average?
With a single treatment of debridement and cautery, approximately 80% of indolent ulcers heal within one to two weeks. The remaining 20% may require more than one treatment and, on occasions, it can take several weeks until full healing of an indolent ulcer is achieved.
The option of surgery for an indolent ulcer may have to be reconsidered if it fails to heal after several attempts at debridement and/or keratotomy.
What complications can occur if my pet has an indolent ulcer?
The biggest concern is certainly the possibility of infection. This can occur even if a suitable broad spectrum antibiotic is used on a preventative basis. If infection occurs, indolent ulcers may become deep and may require urgent surgical intervention.
Until healing of the indolent ulcer is achieved, it is advisable that the patient returns to the surgery to ensure satisfactory progress. Once the ulcer has fully healed, patients should not require frequent veterinary attention and a return will only be necessary in selected cases or if the problem recurs in either eye.
Pet of the month – July – Elsa
by Hannah Wright on July 9th, 2018
Category: Pet of the Month, Tags:
We are so pleased to report that delightful Elsa is making good progress after a very severe bout of Haemorrhagic Gastroenteritis (HGE).
Elsa’s symptoms were initially intractable vomiting. As she did not respond to therapy and has a habit of eating wood which can be very hard to detect on imaging, she underwent an exploratory operation to check that she had not swallowed any. This might in turn have splintered, perforated the bowels and caused peritonitis. Thankfully this did not prove to be the case, however did develop haemorrhagic diarrhoea. Appropriate and swift therapy has put her on the road to recovery!
Pet of the month – June – Bertie
by admin on June 1st, 2018
Category: Pet of the Month, Tags:
What possessed Bertie, at 19 years of age, to change the habits of a lifetime and consume some glass nobody will ever know, but luckily his owner was at hand and observed this.
She quickly rushed him in to the surgery, where radiographs confirmed the presence of 3 pieces of glass in his stomach. Despite worries over his age Bertie underwent an exploratory laparotomy under general anaesthesia to locate and remove the glass.
We are delighted to report that Bertie is doing really well and has bounced back to health!
Healthcare advice for pets travelling abroad
by admin on June 1st, 2018
Category: News, Tags:
When taking your pet abroad it is important to realise that there are potential disease risks which need to be considered. Animals from the UK will have no natural immunity to several diseases which are common in Europe and elsewhere.
The four main disease risks are Leishmaniasis, Babesiosis, Ehrlichiosis and Heartworm. All are potentially life-threatening and so must be carefully considered before travel. These diseases are all transmitted to pets when they are bitten by an infected insect (an insect which spreads a disease in this way is known as a vector). Different insects, or vectors, spread different diseases. With the exception of Heartworm, the only way to protect your pet from catching the disease is to prevent it being bitten by the vectors. Therefore, it is useful to know the feeding habits of the vectors and where they are likely to be found. The tables below give information about these diseases and their insect vectors.
The lists of geographical areas mentioned in the tables are not exhaustive. Also, high-risk times of day or year may be noted in the tables, but vectors will also feed outside these peak times. These diseases principally affect dogs, but cats may also be affected.
Whenever you are travelling abroad with your pet it is sensible to seek the advice of a local veterinary surgeon with regard to preventative health, as he or she will best know the local disease risks. If your pet falls ill while you are abroad you should seek veterinary assistance as soon as possible. It is worth finding out about local vets in the area before travelling, especially if the language is going to be a problem.
Should your pet fall ill after you have returned to the UK, do remember to mention to your veterinary surgeon that your dog or cat has travelled or lived abroad, even if it was years previously, as some of these diseases can take many years to emerge.
Leishmaniasis:
Cause of Leishmaniasis
- Protozoal Parasite
Vector
- Phlebotomine Sandfly
Where do Sandflies live?
- Woods and gardens (not beaches!)
- Mediterranean countries and islands
Feeding activity of Sandflies
- Potentially any time of day
- Peak activity May to October
Prevention of bites
- Do not allow dogs to sleep outside. Sandflies enjoy similar cool resting places to dogs!
- Allowing animals to sleep upstairs may reduce bites, as Sandflies have limited flight
- Environmental insect repellents – e.g. coils and plug-ins
- Scalibor repellent collar for dogs or Advantix
The speed of onset of illness
- It may take up to 6 years for signs to develop after an animal has been bitten
Clinical signs of illness
- Chronic or recurrent weight loss, skin and eye lesions, lameness and enlarged lymph nodes
Treatment
- Variable success of treatment
Special considerations
- Zoonosis (i.e. it can potentially be passed to humans)
Babesiosis:
Cause of Babesiosis
- Protozoal parasite of the red blood cell
Vector
- Tick
Where do Ticks live?
- Forest and rough grazing including campsites!
- France, Southern Europe but as far north as Belgium, Germany and the Netherlands
Feeding activity of Tick
- Especially Spring and Autumn
Prevention of Tick bites
- Prevent tick attachment – repellent collars (Scalibor for dogs)
- Treatments to kill attached ticks – Frontline (cats) or Advantix (dogs)
- Daily checking and removal of ticks using Tick Hook (see note below)
Speed of onset of illness
- Rapid onset disease is possible
Clinical signs of illness
- Due to haemolyticanaemia (destruction of the red blood cells). Pale mucus membranes, jaundice, weakness, fast breathing, red urine, collapse, death
Treatment
- May not be curative
Ehrlichiosis:
Cause of Ehrlichiosis
- A rickettsial parasite in the white blood cells
Vector
- Tick
Where is this Tick found?
- France, Corsica, Spain, Italy and Portugal, and further north to Germany, Belgium and Holland
Feeding activity
- As for Babesiosis
Prevention
- As for Babesiosis
Speed of onset of illness
- Rapid onset disease, sub-clinical infection (i.e. the parasite is in the body but does not cause signs of illness) or chronic infection (i.e. causing a slower, long term illness) are all possible
Clinical signs
- Fever, anorexia and enlarged lymph nodes
Treatment
- Vets most commonly prescribe the antibiotic doxycycline to treat ehrlichiosis in dogs. It is typically given once a day for three to four weeks. Other medications can also be used when the situation warrants.
If a dog receives treatment in a timely manner, his condition will usually begin to improve rapidly, often within just a day or two, and the prognosis for complete recovery is good. In more severe cases, additional treatments (e.g., intravenous fluids, blood transfusions, immunosuppressive medications, and/or pain relievers) may also be necessary.
Heartworm (Dirofilariasis):
Cause of Heartworm
- Nematode worm found in pulmonary arteries (those in the lungs) and heart
Vector
- Mosquitoes
Where do the Mosquitoes live?
- From northern France south to the Mediterranean. Much of the USA and Canada
- Hyper-endemic in the Po Valley in Italy
Feeding activity of Mosquitoes
- Mainly at night but some species feed during the day
- Especially from May to September
Prevention of Mosquito bites
- Small mesh nets or window covers
- Environmental insect repellents – coils and plug-ins
- Scalibor repellent collar for dogs and Advantix
Prevention of disease
- Drug prophylaxis (preventative treatment) using Milbemax tablets – start a month before exposure, then give monthly until one month after return to the UK. Where dogs may have been previously exposed, testing is required prior to treatment. Testing comprises blood tests and chest X-rays (radiographs)
Clinical signs
- Associated with respiratory disease and heart failure
Treatment
- Dogs with heartworm disease will initially receive treatment needed to stabilise their condition. They will then be given medication to kill circulating microfilariae, and most will undergo a series of three injections over a month’s time to kill adult worms in the heart and lungs. Hospitalisation when these injections are given, and possibly at other times, is necessary so that your vet can watch closely for side effects. Prednisolone and doxycycline are also typically prescribed to reduce the chances that the dog will react badly to the death of the worms. Other treatments may be needed based on an individual dog’s condition.
If a dog has caval syndrome, a surgical procedure will be necessary to remove adult worms from the right heart and pulmonary artery by way of the jugular vein. Most dogs with caval syndrome die regardless of treatment.
Summary General Recommendations:
Ticks
Prevent tick attachment
- Scalibor collars (dogs)
- Advantix spot-on (dogs)
Kill Ticks
- Frontline (cats)
- Advantix spot-on (dogs)
Daily check for ticks and remove any found using a Tick Hook
Sandflies and Mosquitoes:
- Keep your pet inside at times of peak activity
- Use meshes/netting over windows
- Use environmental repellents
- Scalibor collar (dogs) or Advantix (dogs)
Heartworm prevention:
- Monthly Milbemax tablets or fortnightly Advocate
- Start one month before exposure and continue until one month after return
Please note:
It is important to take great care when removing ticks to ensure that the mouth parts are fully removed. Failure to do so may cause an abscess or granuloma (inflamed lump) to develop. To ensure safe removal we recommend using a specially designed Tick Hook. These come with instructions for safe tick removal.
All of the above products can be supplied by our clinic. Please note that for licensed veterinary products to be dispensed, your pet needs to be under our care which may require a clinical examination if we have not seen your pet for some time.