News
Archive for January, 2019
Special offer – January 2018
by admin on January 2nd, 2019
Category: Special Offers, Tags:
Pet of the month – January – Brooke
by admin on January 2nd, 2019
Category: Pet of the Month, Tags:
Pet of the month for January is Brooke, a 9 year old Jack Russell Terrier cross, who has suffered from Diabetes Mellitus since last August. We are delighted to report that she is doing very well and has just been into the clinic for one of her regular monitoring appointments called a ‘blood glucose curve’ (see below).
What is Diabetes Mellitus (Sugar Diabetes)?
Most of the food that animals eat is turned into sugars to provide energy for the body. The sugar in the blood then needs to get into the cells of the body to help them work. A hormone called insulin, which is produced by the pancreas (an organ in the tummy near the stomach), helps the sugar to get into the cells. Diabetes develops when the body does not produce sufficient insulin. Insulin regulates blood sugar levels, and when the insulin levels are too low, blood sugar (glucose) levels increase, resulting in diabetes. Diabetes is a potentially life threatening illness, but fortunately it is one which we are able to treat successfully in the majority of cases.
Diabetes occurs most commonly in older dogs, and in middle-aged overweight cats. Some dogs and cats develop diabetes when they are younger, because they have a genetic predisposition for the condition.
What are the signs of Diabetes?
- Increased thirst
- Increased frequency and/or volume of urination
- Possible increased appetite
- Possible weight loss
- Possible smelly urine – because of the presence of ketones (see below) or infection
- Possible lethargy/tiredness
How is Diabetes diagnosed?
Diabetes is diagnosed by careful assessment of the patient’s history and a physical examination, followed by blood and urine tests. Excessive levels of sugar in the urine and blood are highly suggestive of diabetes, although occasionally a sick or anxious patient may have increased sugar levels as a result of stress (such as visiting the vets!). If there is some doubt about the significance of a single high blood and urine sugar result, we may perform a special blood test (fructosamine) which gives us an indication of the blood sugar levels over several previous weeks.
When a patient is diagnosed with diabetes, we often look for underlying causes of diabetes such as obesity, Cushing’s syndrome (a steroid hormone imbalance), pancreatitis (inflammation of the pancreas – the organ that produces insulin) or previous administration of some medications. If we find any of these underlying problems, they also need to be managed alongside the diabetes.
What effects does diabetes have?
Diabetes leads to a build up of sugar in the bloodstream and in the urine, and not enough sugar can actually get from the blood into the tissues that need sugars to work properly. This leads to widespread effects on the body, including urinary tract infections, kidney disease, liver disease and eye disease.
If diabetes is left untreated or poorly controlled, the body is starved of glucose-based energy supplies, and the body reacts by using up protein and fat stores for energy instead. Protein stores can be converted to glucose, but using up stored fat leads to the production of substances called ketones. A build up of ketones can lead to a very serious condition called Diabetic Ketoacidosis (see later) – this is a medical emergency requiring intensive care.
How is Diabetes treated?
Diabetes is best treated with insulin. In most cases, insulin is administered as an injection under the skin twice a day. There are also tablets that can be used to help regulate blood glucose levels, but these are not the best way of treating the condition.
Although owners are often concerned about giving injections to their pet, most dogs and cats are very amenable to being given injections. If your pet is diagnosed with diabetes, we will spend as much time as is necessary to teach you how to give insulin injections and how to look after the insulin and syringes.
There are several types of insulin, and the dose of insulin is very individual. It is very important that you do not change the dose of insulin without instructions from your veterinary surgeon. Most dogs and cats need a little modification of the doses of insulin with time, and these changes will be made based on monitoring and blood tests. You may be instructed on how to monitor blood or urine glucose/ketone levels at home. Urine should be checked regularly for the presence of ketones, as the presence of these for two or more days can indicate a complication of uncontrolled diabetes – Diabetic Ketoacidosis (see later).
Care and use of insulin:
It is important that affected dogs continue to exercise regularly as this will help to keep their weight down. Also exercise has also been shown to make insulin work better, resulting in better stability of the blood sugar levels.
- Diet - In addition to insulin, it may be important to modify your pet’s diet, particularly if your dog or cat is overweight, or has inflammation of the pancreas (pancreatitis) in addition to diabetes. These dietary changes will be directed by your veterinary surgeon. Once stabilised, dogs and cats are fed just before the insulin is administered, to make sure that they have eaten before the insulin is given. We have a full-time veterinary nutritionist who can be consulted regarding the specific dietary needs for your pet.
- Exercise - It is important that affected dogs still exercise regularly. This helps them to maintain a healthy weight, and it helps to keep the blood sugar more stable.
How quickly does the treatment work?
- Don’t expect a quick fix. It can be very difficult to regulate the blood sugar in some diabetics. Even in the best situation, it will take several weeks, including check-ups and blood tests, before your pet’s diabetes can be stabilised. It is important to discuss any concerns you have about giving insulin with your vet at any check-up. We may ask you to show us how you are storing insulin and administering it, should control be proving difficult.
Some medications (such as steroids e.g. prednisolone), hormones (such as progesterone) and diseases (e.g. infections such as tooth and gum infections) will interfere with insulin’s action in the body. Any additional medications that your pet is having should be discussed with your veterinary surgeon prior to use. Because hormones affect the action of insulin, it is important that entire female bitches are neutered (spayed) to help to control their diabetes.
What is a ‘hypo’ episode (hypoglycaemia)?
Hypoglycaemia is a low blood sugar level. This occurs when too much insulin for the amount of food eaten results in too little sugar circulating in the blood. This most often occurs when a pet does not eat and still has insulin given, or is accidentally given a higher than normal dose of insulin (most often because the insulin is given twice, by mistake). Low blood sugar levels will make the affected animal very weak, and this can result in collapse or twitchiness and seizures (fits). If you are ever concerned that you have given your pet too much insulin, or that you have given insulin and your pet has not eaten, or has vomited up his or her food, please contact us.
How to monitor your pet’s diabetes at home
There are many features you can measure or observe at home to help to monitor your diabetic pet:
- Amount of water being drunk
- Frequency and volume of urination
- Appetite – how much is eaten?
- Body weight
- Behaviour
- Presence of ketones/glucose in your pet’s urine (using a special dipstick that you put into the urine)
It is very helpful to make a diary with this information in it, and provide it to your vet at every check-up.
Follow-up consultations are performed frequently (the frequency depends on the individual patient). These follow-up visits may include a single blood test (fructosamine), or they may be followed by admission of your pet into hospital for the day for a ‘blood glucose curve’. A blood glucose curve involves us performing several small blood tests throughout the day, and plotting the results on a graph (making a ‘curve’ on the graph). This allows us to see how your pet’s blood glucose changes throughout the day which can be useful for adjusting your pet’s food intake and insulin dosing regime.
What are the possible complications of diabetes?
- Cataracts – cataracts are changes in the lens inside the eye which can lead to blindness. Many dogs develop cataracts within 6 to 12 months of developing diabetes. Specialist treatment is available, and the majority of diabetic patients do very well after cataract surgery. Diabetic cataracts do not tend to develop in cats unless the diabetes occurs when they are very young • Retinal disease – degeneration of the sensitive area at the back of the eyes
- Neuropathy – disease of the nerves causing weakness
- Nephropathy – kidney disease
- Infections – it is common for diabetic patients to develop infections, especially of the urinary tract (bladder and kidneys)
- Ketoacidosis – in cases of uncontrolled diabetes, toxic (poisonous) metabolites (natural break-down chemicals) are produced which can lead to illness, lethargy, coma and death
The better the stabilisation of the patient, the better these complications are likely to be controlled or prevented.
What is the long term outlook?
Diabetes can be a very rewarding condition to manage. Most pets are very amenable to treatment, and diabetic animals can have a very good quality of life. Diabetes in cats can be temporary, and affected cats may only require insulin administration for a limited time (often 3 to 6 months) provided that the underlying cause, such as obesity or pancreatitis, is removed. Many dogs with diabetes eventually develop cataracts and these can cause quite rapid onset blindness. Fortunately most diabetic dogs with cataracts are good candidates for surgery, and Specialist eye vets are very experienced in treating cataracts.
Patients should be reassessed at regular intervals set by your veterinary surgeon. Pets that are having insulin treatment should also be reassessed if they:
- become unwell
- are losing weight
- have a change in appetite
- have excessive thirst or urination
- become weak, wobbly or disorientated (this can be an emergency due to hypoglycaemia or severe diabetic ketoacidosis – see above)
- have ketones in their urine for more than 2 consecutive days
If you have any concerns about your diabetic pet please do not hesitate to contact us.
Canine Demodicosis
by admin on January 2nd, 2019
Category: News, Tags:
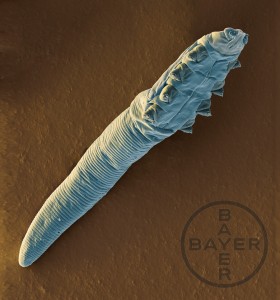
What are Demodex mites? And what is demodicosis?
Demodex spp. are cigar shaped microscopic parasitic mites that live within the hair follicles of all dogs. These mites are passed to puppies from their mothers in the first few days of life, and then live within the hair follicles for the duration of animal’s life without causing problems. It is thought that the body’s immune system helps to keep mite numbers ‘in check’ and prevent the populations getting out of control. For the vast majority of dogs, these mites never cause a problem. However in some instances, mite populations become huge resulting in inflammation and clinical disease. This disease is called demodicosis.
What causes demodicosis?
There are two presentations of demodicosis depending on the age at which it develops. Juvenile onset demodicosis tends to occur in puppyhood between the ages of 3 months and 18 months, and occurs in both localised and generalised forms. The exact cause is quite poorly understood but probably occurs due to a mite specific genetic defect in the immune system which allows mite numbers to increase. This defect may or may not resolve as the puppy ages. It is thought to be ‘mite specific’ because these puppies are healthy in all other respects and do not succumb to other infections. Generalised demodicosis can be a very severe disease. Adult onset demodicosis usually occurs in the generalised form and in dogs over 4 years of age. It is generally considered a more severe disease than its juvenile onset counterpart. In these cases, mite numbers have been controlled in normal numbers in the hair follicles for years prior to the onset of disease, which tends to result from a systemic illness affecting the immune system. Common triggers for adult onset demodicosis include hormonal diseases and cancer.
What are the clinical signs?
Localised demodicosis in juvenile dogs presents as patches of hair loss and red inflamed skin. These patches often occur around the face, head and feet and are not typically itchy.
Generalised disease in juvenile and adult dogs is a more serious disease, although there is no uniformly accepted way of defining the number of lesions needed to classify generalised disease. Patches of hair loss and inflammation develop which often coalesce into large areas of thickened skin and sores. As the parasites damage the hair follicles, secondary bacterial infections are very common and affected dogs can develop discharging lumps within the skin. Bleeding from these lesions is not uncommon. As with the localised form, lesions often start around the head, face and feet, but often spread to involve large areas of the body surface. The ears can also be affected with this parasite, resulting in secondary infections. Itchiness and pain are commonly seen.
How is it diagnosed?
Demodicosis can often be suspected following a review of the animal’s history and assessment of the clinical signs. The parasitic mites within the hair follicles result in plugging and the formation of ‘black heads’. The plugged follicles also cause large amounts of scale to be present on the hairs themselves. Demodicosis can usually be diagnosed relatively easily. Hairs can be plucked from the affected skin and then examined under a microscope for the presence of the mites. Alternatively, the skin can be squeezed and then scraped with a blade to collect up the surface debris from the skin. This material is then also examined under a microscope for the parasites.
If the numbers of mites are abnormal and if mites can be recovered from multiple sites, demodicosis can be diagnosed. Rarely, a biopsy of affected skin is needed to diagnose the condition.
Is it contagious?
Demodex mites from dogs are considered non-infectious to in-contact animals and people. It is thought that Demodex mites can only be passed between dogs in the first few days of life from the mother to the pup.
How is it treated?
The treatment used for demodicosis depends on the age of the animal and the severity of the disease. Mild and localised forms of demodicosis in young dogs may not require treatment, and may resolve spontaneously as the animal ages. These cases should be closely monitored if no treatment is given. Generalised cases in young dogs and those in adult dogs require intensive treatment. Secondary infections must be treated with courses of antibiotics, and a swab is often submitted to a laboratory to grow the organisms to ensure the correct antibiotic is selected. The licensed treatments for demodicosis in the UK include a dip solution called Aludex and a spot-on product called Advocate. The dip is performed on a weekly basis until mite numbers are brought under control. Advocate spot-on is generally used for milder cases and is usually used monthly. In severe cases not responding to the licensed treatments, off-licence treatments must be used. Some of these drugs, such as Ivermectin and Milbemycin, are used for demodicosis in other countries.
An essential part of treating adult onset cases is to identify the underlying illness that triggered the problem. This often requires blood testing and scans (CT, ultrasound) to investigate.
Treatment must continue until mite numbers have returned to a normal level and this can take a very long time. This can only be assessed by repeat sampling of the patient using plucks of the hair or scrapes of the skin
What is the prognosis?
The prognosis for localised disease in young dogs is very good, and most recover uneventfully from the disease. Generalised cases in young dogs can take many weeks or even months of treatment, but it is usually possible to control the disease with a good long term outlook.
The prognosis for adult onset generalised demodicosis is far more uncertain, as many of these dogs have an underlying systemic illness. If this illness can be identified and cured, the prognosis for managing the demodicosis is much better. Some cases require long term medication to keep mite numbers controlled.