Archive for the ‘News’ Category
by on October 31st, 2014
Category: News, Tags:
Canine Prostate Awareness Month
Canine Prostate Awareness Month (CPAM) is an initiative to highlight the prevalence of Benign Prostatic Hyperplasia (BPH) in male dogs, and to encourage owners to check for and seek treatment for it. CPAM takes place during November – or ‘Movember’ as it has been called by those fundraising for human male prostate disease and testicular cancer.
More than 80% of entire male dogs over the age of five suffer from BPH, a painful condition which is often hidden.
CPAM aims to remind us that men are not the only ones to suffer from prostate disorders. It’s a well-supported initiative and, running it at a time when the media spotlight is already on the dangers of prostate cancer in men, means we can spread the message that owners should also be monitoring dogs for signs of prostate disease. The problem with BPH is that the majority of dogs suffer in silence. It is a painful condition that too often goes unnoticed until it reaches an advanced stage, where the owner notices blood in the urine or painful urination.
Clinical signs of Prostate disease include:
- Straining to pass faeces (due to size of prostate)
- Straining to pass urine/ no passage of urine
- Blood present in urine
- Stiff hind limb movement.
If you are concerned at all about your dog showing any of the above signs please contact the surgery to make an appointment.
Diagnosis and monitoring of BPH is carried out via blood tests and rectal palpation. Simple medical treatment can be administered, the effects of which can be seen within a week and last for six months.
by on September 30th, 2014
Category: News, Tags:
Firework stress affects almost 50% of dogs and many cats too.
 With November fast approaching now is the time to take appropriate steps to alleviate a potentially distressing time for your pet.
With November fast approaching now is the time to take appropriate steps to alleviate a potentially distressing time for your pet.
Stress can manifest itself in many ways – some dogs will run around and vocalise; others even become destructive and may harm themselves. However, sometimes the signs of stress can be much more subtle. This is especially true for cats and they will often withdraw and hide, meaning that their stress is not easily recognised
The most important change that must be made is for you to change your behaviour. It is completely natural to want to reassure your pet when it is stressed however all this does is reinforce the unwanted behaviour and unfortunately makes matters worse.
If stress associated with fireworks is not dealt with, it often progresses to fear of other sounds like thunder and gunshots and eventually even every day noises such as car doors slamming. As a result we must address this problem promptly and effectively to improve the welfare of our pets.
Managing firework stress needs an approach to both the short and long-term issue. In the short term we must manage our pets on the night. Long term we need to change the feelings our pets associate with fireworks in order that they do not become stressed.
Short Term Management
Here are some useful tips to help your pet cope during the firework season:
* Provide a den or hiding place and ideally where your pet would normally seek refuge
* Muffle the sound of the fireworks and radio, television, close the curtains
* Keep your pet inside and close the cat flap and ensure you dog is not able to access the garden
* Do not fuss them, or tell them off, if they are stressed
* Reward quiet, calm behaviour
* Consider anxiety relieving products such as Adaptil, Feliway, Zylkene and KalmAid. There are no known side effects with these products such as sedation or memory loss. They can be used for both short and long-term management.
Long Term Management
Sound desensitisation is proven to address the underlying problem by altering your pet’s reaction to the stress-inducing noises. It works by exposing your pet to the scary sounds under controlled conditions whilst it is doing something enjoyable such as chewing a favourite toy or treat. This then breaks the negative association that your pet has learned with respect to fireworks and makes the association more positive. The most common method uses CD’s which are played initially for a very short amount of time at low volume. The length of time and volume is gradually increased as your pet progresses through the programme.
Sound Desensitisation takes time (usually weeks to months) and you must be guided by your pet as to how quickly you can progress.
How do anxiety-relieving products help?
Zylkene is a novel natural product derived from milk protein, which has relaxing properties, and is proven to help manage stress in cats and dogs.
KalmAid contains L-Tryptophan which is an essential amino acid that affects production of serotonin. Serotonin has a calming and relaxing effect. L-theanine, another amino acid also has a calming effect. Vitamin B1 is added as deficiency has been associated with nervous disorders.
Feliway is a synthetic copy of the natural feline facial pheromone, and creates a state of familiarity and security in the cat’s local environment.
Adaptil is a copy of a naturally released dog ‘appeasing pheromone’ that has a comforting and reassuring influence.
Please make an appointment to discuss your pet’s specific needs with us.
by on September 1st, 2014
Category: News, Tags:
An Emerging Respiratory Disease That Can Kill
The Canine Infectious Respiratory Disease (CIRD) Group at the Royal Veterinary College (RVC) are currently researching a bacterial disease that has been increasingly implicated in fatal cases of infectious pneumonia in dogs over the past five years. They are calling for dog owners and vets to recognise the signs of the potentially fatal disease Streptococcal pneumonia to ensure rapid treatment and contribute to research to reduce further spread.
The bacterial infection Streptococcus zooepidemicus causes a severe, bloody pneumonia in dogs, producing signs similar to those associated with toxic-shock syndrome in humans.
How is Streptococcus zooepidemicus transmitted?
The bacterium can be ‘carried’ by dogs in their upper respiratory tract (most likely their tonsils) without showing any symptoms of disease and it is likely that, as yet unknown, bacterial, host or environmental factors, possibly including an over-exuberant immune response to the bacteria, are responsible for the severe pneumonia observed in the worst cases. These ‘carrier’ dogs may be an important source of infection if introduced to new populations, especially in rehoming kennels where dog come and go all the time.
What are the signs of Streptococcal pneumonia in dogs?
Infected dogs develop the following signs:
Sudden-onset fever
Sneezing
Rapid, shallow breathing
Bloody discharges from the nose or mouth
Lethargy (tiredness)
Reluctance to eat
Some dogs may collapse, which indicates a developing septicaemia. In most cases this occurs within 12-24 hours of the onset of the first symptoms (which may be mistaken for classical ‘kennel cough’ caused by viruses). In a small proportion of cases, the disease has been known to be fatal to dogs within 24 hours of contracting the infection.
How likely is the disease to occur in pet dogs?
In most cases there seems to be a trigger-factor such as a significant stressful event, for example rehoming, strenuous activity such as a race, or preceding illness. Outbreaks are isolated and tend to occur where dogs mix in large groups. Although it is rarer in family pets, it is still important for owners to be aware of the symptoms, especially if they regularly visit kennels or go to events where animals gather. In the initial stages, signs are similar to those of the more common ‘kennel cough’, which occurs in similar environments. However, in Streptococcus zooepidemicus outbreaks, dogs quickly become seriously ill and show very severe signs. In contrast, most dogs with kennel cough will usually have a relatively mild illness and deaths are rare.
Can pneumonia caused by Streptococcus zooepidemicus be treated?
Treatment of Streptococcal pneumonia is often ineffective unless started rapidly following onset of the first symptoms and is currently based on a suspected diagnosis. If owners notice the sudden onset of a fever in their dog, accompanied by sneezing, nasal discharge which is often bloody, and their animal becoming lethargic, they are advised to seek veterinary help immediately. With prompt identification, medical treatment and supportive care, dogs can make a full recovery.
by on August 4th, 2014
Category: News, Tags:
 The most unexpected things around the home and garden can present a hazard to your pets. This week we look at ten unexpected dangers you might not have been aware of. Prevention is better than cure – if you can, always ensure that potential hazards are kept securely away from your animals, and take what steps you can to prevent exposure. If you suspect your pet may have eaten or encountered any of the hazards discussed in this newsletter, contact your vets straight away for advice and appropriate treatment; do this even if your pet seems completely well, as with many of these dangers, there can be a delay of hours to days before signs of illness become apparent. Starting treatment before the pet starts to appear unwell can significantly improve the odds of them making a full recovery.
The most unexpected things around the home and garden can present a hazard to your pets. This week we look at ten unexpected dangers you might not have been aware of. Prevention is better than cure – if you can, always ensure that potential hazards are kept securely away from your animals, and take what steps you can to prevent exposure. If you suspect your pet may have eaten or encountered any of the hazards discussed in this newsletter, contact your vets straight away for advice and appropriate treatment; do this even if your pet seems completely well, as with many of these dangers, there can be a delay of hours to days before signs of illness become apparent. Starting treatment before the pet starts to appear unwell can significantly improve the odds of them making a full recovery.
Raisins
Raisins contain an as-yet unidentified substance which can in some cases cause acute renal (kidney) failure in dogs. And it’s not just raisins, but currants, sultanas, and even fresh grapes, too.
Raisins and grapes are a rather unusual poison, as some dogs seem to be able to eat them quite safely – whereas other dogs can develop life-threatening acute kidney failure; as few as four or five grapes are believed to have resulted in one dog’s death. The mechanism of the toxic effect is still unknown, and since there’s no way of really knowing whether your dog is going to be one of the unlucky ones, it’s best to make sure they never eat any kind of grapes, raisins, or other dried vine fruits – whether they’re raw, or prepared in cakes, puddings or other cooking. Christmas, with its proliferation of mince pies, Christmas pudding and other seasonal treats, is a particularly high risk time of year!
Painkillers
Just about all of us have a pack of Paracetamol, Ibuprofen, or Asprin somewhere around the house (and often in our handbags, too!). While they are freely available without prescription, and very widely used by people, all of these medicines (from a family known as the non-steroidal anti-inflammatory drugs) have the potential to cause illness in our pets, sometimes even after only a very tiny dose.
The toxic effects can vary quite widely depending on the drug taken, and the species of animal, and include the potential development of stomach ulcers, liver and kidney damage, and also abnormalities affecting the blood. Confusingly, these medicines are sometimes used intentionally in dogs and cats by veterinary surgeons – they can be very useful, powerful drugs, if used carefully and in appropriate patients. If you ever find a chewed up pill packet (whether it contained over the counter painkillers, or any other medication) contact your veterinary surgery ASAP for advice.
Cut flowers
All the parts of lily plants (including the pollen which is present on the stamens of lilies in cut flower arrangements) are highly poisonous to cats, with the potential to cause life threatening kidney failure. Cats can be harmed even as a result of swallowing pollen which has transferred to their fur while walking past flowering lilies, or from chewing leaves or flowers, either from flower arrangements, or from plants growing outdoors in gardens
Fortunately general awareness of this problem is now growing, and cut flower arrangements containing lilies – particularly those from larger retailers – are starting to carry warning labels. Plants and cut flowers from the Lilium and Hemerocallis species are most hazardous, though other lily-type flowers (including lily-of-the-valley) also present a variety of different toxic hazards.
Bread dough
Bread dough is an occasional cause of serious illness and can affect all species, though dogs, due to their tendencies to eat all kinds of things, are most often affected. Dough containing live yeasts will continue to ‘rise’ (that’s to say increase in volume) inside the dog’s stomach, which is at more or less a perfect temperature! Because of the elastic, springy nature of rising bread dough, it tends to stay in a large ball and is extremely difficult for the dog to vomit up or to pass further down the digestive tract.
As the ball of dough swells, it stretches the stomach wall, causing pain, and serious damage to the tissue as a result of the blood supply being compromised – very much as happens during the life-threatening condition GDV (gastric dilatation and volvulus, or ‘bloat’). As if this wasn’t bad enough, the yeasts also produce alcohol (ethanol) as a by-product of their fermentation, and this can be enough to cause symptoms of alcohol toxicosis. So, keen bakers among you, keep your rising dough and proving loaves safely out of reach of your pets!
Certain over-the-counter flea products
A number of over-the-counter flea spot-on products marketed for dogs in the UK and elsewhere in the world contain an active ingredient from the pyrethrin or pyrethroid family (most commonly ‘permethrin’). While these are generally well tolerated by dogs, the concentration of active ingredient in these products can potentially make for a lethal dose for a cat, whether the product itself is accidentally applied to the cat in error, or even due to cats snuggling up to recently treated dogs in the household and the product rubbing onto them.
Cats exposed to permethrin develop twitches and muscle tremors which can progress to epileptic-type fits if the drug passes into their brain and central nervous system in a high enough concentration. These seizures can sometimes be fatal. To be on the safe side, contact your veterinary surgery for advice on appropriate safe flea products for your whole household.
Needles & threads
Most cats just can’t resist string or thread, which is a habit that can get them into trouble! Playing can sometimes lead to biting and swallowing, and swallowing string (or sewing thread, knitting yarn, ribbon, tinsel…) can cause a very serious form of foreign body obstruction in the gastrointestinal tract, which can require extensive surgery to resolve, and can sadly sometimes lead to the death of the patient. Unfortunately, sometimes the threads that cats find have sewing needles on the end of them, which can complicate matters further, increasing the risk of gut perforation and problems associated with needle migration. Kittens, who are particularly inquisitive and playful, are especially at risk, so keep your needles and threads safely locked away!
Corn on the cob
Dogs seem to love to chew on these, and if they swallow a piece, corn cobs seem to be almost the perfect size to cause an obstruction in the intestines. Unlike some of the other unfortunate non-food items our dogs like to chew on and sometimes swallow, corn cobs are essentially invisible on x-ray, which can make the process of identifying and diagnosing the foreign body obstruction even more challenging than usual for veterinary staff.
Classic opportunities for dogs eating corn cobs are at summer family BBQs – other BBQ party hazards include cooked bones, and kebab sticks – and scavenging in bins. Yet another reason to ask visitors to your home not to feed your dogs tit-bits, and keep your kitchen waste secure until bin day!
Cement powder
Powdered cement and concrete, both before use, and the dust produced from cutting or grinding solid materials, can pose a serious hazard to fish and waterways. Cement powder is a strong alkali, and when added to water can raise the pH very substantially, exposing any animals in that water to the risk of what are, essentially, chemical burns. In addition, the fine powder easily clogs the gills of fish, and can suffocate them rapidly.
If you’re having building work (or there is some going on nearby) it’s really important to cover and protect both outdoor ponds and indoor fish tanks if there is any risk of cement or concrete debris contaminating them. And, since many surface water drains flush into waterways with minimal water treatment, anyone working with cement or concrete should avoid washing any wastes ‘away’ into surface drainage, as dilution does very little to reduce the hazard, and serious damage can be caused to river and lake ecosystems as a result of cement and concrete run-off.
Antifreeze
Vehicle antifreeze (ethylene glycol) can cause poisoning in all animals, but most commonly affects dogs and cats. Ethylene glycol tastes sweet, which is attractive to pets, and unfortunately vehicle antifreeze is often stored very insecurely in sheds and garages, and not cleared up carefully after accidental spills or leaks from car radiators. The lethal dose of undiluted antifreeze solution in a cat could be as little as a teaspoon.
Symptoms initially resemble drunkenness, with balance and movement abnormalities, and often vomiting. As the ethylene glycol is metabolised in the body, substances are created which cause serious and irreversible damage to the tissues of the kidneys, resulting in rapid kidney failure. Pets who have consumed antifreeze unfortunately often do not survive, but time is of the essence and the sooner treatment is started the better the odds. So check around your home, and any sheds, garages and outbuildings for antifreeze and make sure it is stored correctly, and if you ever suspect antifreeze poisoning in your pets, act fast.
Curtains
It is common, particularly in more expensive hand-made curtains, to use small weights, either in the corners of the bottom hem, or all along the bottom hem, to help the curtains hang nicely. These weights are still very often made of lead.
These little nuggets can look like an object of interest to small mammals – including rabbits – and pet birds, especially parrots with their inquisitive natures, to whom they resemble nuts or seeds. If swallowed, they can cause lead poisoning. The other common cause of accidental lead poisoning in small pets and birds is the use of previously painted wood to make hutches, runs, and similar structures – if this wood is old enough to have been treated with lead paint in the past, very little may be required to cause serious health problems.
by on July 2nd, 2014
Category: News, Tags:
 Many of us value our hens like our other family pets and want to be able to get professional advice and treatment if they fall ill. Currently most vets get minimal training on backyard chicken diagnosis and care, but with increasing numbers of hens now being kept across the country because of our re-homing initiative, there is a growing demand for specialist knowledge and treatment.
Many of us value our hens like our other family pets and want to be able to get professional advice and treatment if they fall ill. Currently most vets get minimal training on backyard chicken diagnosis and care, but with increasing numbers of hens now being kept across the country because of our re-homing initiative, there is a growing demand for specialist knowledge and treatment.
Although Fitzalan House has always been keen to treat poultry, we are delighted to tell you that vet Alison Livesey has recently been on an extensive course run by Chickenvet Poultry Vet Specialists and is able to offer an exceptionally well-informed service.
by on May 30th, 2014
Category: News, Tags:
 Having trouble breathing is, at the very least, an uncomfortable experience, but can also be life-threatening if your pet is unable to take in enough oxygen to their lungs when breathing in, or to get rid of enough carbon dioxide from their lungs when breathing out.
Having trouble breathing is, at the very least, an uncomfortable experience, but can also be life-threatening if your pet is unable to take in enough oxygen to their lungs when breathing in, or to get rid of enough carbon dioxide from their lungs when breathing out.
What can cause difficulty breathing in cats and dogs?
There are lots of different causes of difficulty breathing but most of the time they are due to a problem which affects the airway or the lungs in some way. Some of the disorders which can occur in different parts of the respiratory tract are listed below.
Affected part of airway: nose, throat (pharynx), vocal cord area (larynx):-
- Brachycephalic airway obstruction syndrome is seen in dogs with short-noses such as Pugs and Bulldogs and includes a number of airway abnormalities present from birth. Increased risk on hot days, during exercise or stress
- Laryngeal paralysis – the vocal cords fail to move properly during breathing. Especially larger breed dogs (e.g. retrievers). Increased risk on hot days, during exercise
- Masses causing obstruction – may be cancerous but not always (e.g. nasopharyngeal polyps in cats)
Affected part of airway: windpipe (trachea):-
- Tracheal collapse – the windpipe flattens during breathing hindering airflow. Especially little dogs (e.g. Yorkshire terriers, Chihuahuas) who often have a characteristic cough (‘goose honk cough’); often gets worse when excited or stressed
- Tracheal foreign body e.g. bone or pebble stuck in windpipe
Affected part of airway: lungs:-
- Bruising (contusion) for example after a traumatic episode (e.g. cat hit by car)
- ‘Water on the lungs’ (pulmonary oedema) – especially due to heart failure
- Infection (pneumonia). Especially bacterial infections after inhaling stomach contents (aspiration pneumonia). Also lungworm – especially in dogs
- Cancer – may originate in the lungs or spread there from somewhere else in the body
- Allergy – especially feline asthma (allergic airway disease)
- Foreign body – e.g. inhaled grass awn or other plant material
Affected part of airway: chest cavity around lungs:-
- Build-up of air (pneumothorax) due to airway rupture, especially after a traumatic episode (e.g. cat hit by car)
- Build-up of fluid (pleural effusion) due to e.g. heart failure; infection (pyothorax); bleeding
- Diaphragm rupture – usally after trauma when organs such as the stomach or liver may move into chest
How will I know that my pet is having difficulty breathing?
It may well be obvious to you that your pet is struggling to breathe because you are used to seeing them breathing normally and will notice a change. In many cases there is an increase in both the rate and effort of breathing but one or other may occur. You may notice for example that there is more movement of their chest and tummy area or that there is flaring of the nostrils. Some of the most severely affected animals show ‘postural adaptations’ to help them move air (e.g. sitting upright rather than lying down, standing with their elbows out). In very severe cases, the gums may take on a bluish or purplish appearance rather than their normal salmon pink colour. This is referred to as ‘cyanosis’ and should prompt immediate veterinary attention.
What will my vet do to help my pet?
Your vet may want to approach the management of your pet in a slow and steady fashion, taking their time to do the various necessary tests and treatments rather than risking stressing your pet.
More severe cases receive oxygen therapy and sometimes various drugs straight away to try and make them more stable for further tests and treatments. It may also be necessary, for example, to remove air or fluid from around the lungs using a needle (thoracocentesis). Commonly performed tests include ultrasonography and taking x-rays, and an ECG may be done in some cases where heart failure is suspected to see whether the heart is beating with a normal rhythm. In some cases an endoscope (like a tiny video camera) is passed into the airway under a general anaesthetic and other tests that may be performed include analysing your pet’s faeces and taking blood tests.
Depending on the diagnosis, your pet may need to be on medications, sometimes for the rest of his or her life, or they may need an operation. Their exercise may need to be restricted, sometimes just for a while but sometimes also more long-term. Unfortunately in some cases the cause of the difficulty breathing is one that has a very poor outlook. As there are many reasons why your pet may be having difficulty breathing, it is not possible to be too specific here and you should consult your vet if you are at all worried about your pet’s breathing.
If you are worried about your pet’s breathing you must consult your veterinary practice immediately. Dogs and especially cats that are struggling to breathe are in a very vulnerable position and it is very important to try and stress them as little as possible or they may deteriorate.
by on April 30th, 2014
Category: News, Tags:
 Last year only half of the UK dog and cat population were fully protected against infectious diseases. Was your pet one of them?
Last year only half of the UK dog and cat population were fully protected against infectious diseases. Was your pet one of them?
If it has been over 12 months since you last visited us, then your pet could be at risk of contracting potentially fatal infections such as parvovirus, leptospirosis or cat ’flu. Unfortunately, immunity to these diseases does not last a lifetime and will gradually wane, leaving your pet at increased risk of disease. To ensure continued protection, you need to make sure that they are regularly ‘boosted’ against these diseases.
Vaccination has been one of the great success stories of veterinary medicine, and has saved countless thousands of animals. But these days – thanks, largely, to vaccination – infectious disease is much less obvious; and of course in the UK, the MMR debate seems to have damaged the reputation of vaccines in general.
More recently, there’s been discussion in the media about pet booster vaccinations. Are they really essential to your pets health? Or are they just a way for your vet to make money? It’s worth remembering that many of the pet diseases we vaccinate against are killers. Whereas a child with mumps will almost certainly get better, an unvaccinated dog that contracts parvovirus can easily die. Only vaccination can prevent these diseases in animals exposed to infection. Even those who question the need for annual boosters are strongly supportive of vaccination overall.
Are annual boosters really necessary? Major studies have been carried out to determine whether the annual booster period can be extended. As a result some vaccines, such as rabies, are now licensed to protect pets for up to three years. However, it is vital to realise that for some diseases, protection is much shorter. Especially for leptospirosis in dogs – no vaccine will protect your pet for more than a year – and leukaemia in cats. This is based on real data and studies have shown that even with one of the best vaccines protection starts to decline after about 12 months. So despite significant developmental advances annual boosters are still essential.
Our practice is launching a scheme this November only to help you ensure that your pet’s vaccinations are up-to-date. If your pet’s last vaccination was more than 18 months ago, a restart consisting of a full course of two vaccinations will be necessary to maintain protection. We’re offering owners the opportunity of having a full vaccination course for the price of a booster, saving over 20% on the usual price. In addition, this visit will also enable us to give your pet a full lifestyle health check and identify any other potential health problems at an early stage. Remember, prevention is always better than cure!
To participate, simply speak to our receptionist or ring the surgery to book an appointment and enrol your pet in the scheme, which will only be running until 31st May 2014. Just one step to find out more could ensure your pet stays healthy!
by on March 31st, 2014
Category: News, Tags:
 Ticks are second only to mosquitoes throughout the world in transmitting infectious disease to humans and animals.
Ticks are second only to mosquitoes throughout the world in transmitting infectious disease to humans and animals.
Although the majority of tick-borne diseases in dogs and cats are thought to be exotic to the UK, Lyme disease and Anaplasmosis are already present in the UK, both having the potential to infect not only pets but humans as well.
LYME DISEASE is a bacterial infection that is usually carried by the deer tick. Symptoms include lameness, fever, loss of appetite, fatigue and an abnormal enlargement of the lymph nodes. It is often treatable with antibiotics.
ANAPLASMOSIS is an infectious blood disease that attacks the white blood cells, crippling the immune system. Symptoms include fever, depression, seizures, meningitis, lameness and joint swelling, weight loss, and loss of appetite. It is treatable with antibiotics.
Tick-borne disease is an emerging illness that is often misdiagnosed due to the variety of symptoms, all of which can mimic other conditions. Whilst these symptoms are non-specific and can occur in a variety of illnesses, if your cat or dog displays any of the following warning signs, he/she may have been bitten by a tick:
• Fever
• Lameness
• Loss of appetite
• Sudden onset of pain in their legs or body
• Arthritis or swelling in your pet’s joints
• Lethargy or depression
• Cough
Contact your veterinary surgeon immediately to book an appointment.
In addition please be aware that life-threatening tick-borne diseases such as Babesiosis and Ehrlichioisis can be transmitted to pets travelling abroad, even as close to home as France, therefore regular tick treatment for travelling pets is vital! Call in for advice.
by on February 27th, 2014
Category: News, Tags:

A ‘blocked’ cat describes a patient that can’t pass urine due to an obstruction. It is one of the true emergencies affecting cats and it can quickly become life-threatening (1-2 days). Any cat can be affected but it is much more common in males. It is therefore essential that everyone who lives with a male cat is aware of this condition.
What is a ‘blocked’ cat?
Like humans, cats have two kidneys which make urine by filtering the blood. Urine flows down (via tubes called ureters) from the kidneys into the urinary bladder; it is then excreted from the body through a tube called the urethra which connects the bladder to the outside. ‘Blocked cats’ are ones in which the urethra becomes obstructed preventing urine from being passed. Therefore the correct medical term for this blockage is a urethral obstruction.
Why is urethral obstruction more common in male cats?
In male cats the urethra runs from the bladder through the penis to the outside world. At a certain point there is a bend in the urethra and it becomes narrower; this is the main reason why male cats are much more commonly affected by urethral obstruction. In female cats the urethra is shorter, does not have a bend in it and does not become narrower.
Which male cats are more likely to be affected?
Urethral obstruction can be seen in all kinds of male cats but it is most common in ones that are:
- Overweight
- Confined indoors
- Fed dry food only
Many blocked cats are young or middle-aged and have been neutered – but the problem can occur in older cats and uncastrated ones as well.
What is it that blocks the urethra?
The urethra most often gets blocked by ‘plugs’ of material including protein, cells and little crystals and/or by stones (uroliths) formed from minerals. These substances are usually present in the urine in small amounts but they can build up and then cause an obstruction. This may be more likely in cats that do not consume enough water (either in their diet or by drinking) or that do not urinate often enough. Most blocked tomcats do not have a urinary tract infection.
Other much less common causes of urethral obstruction include tumours and in some cases a cause is not found.
Why is it a problem if the urethra becomes obstructed?
The body needs to be able to pass urine in order to get rid of substances (e.g. potassium, acid) that are harmful when they accumulate in the body. When the urethra gets blocked these substances are not removed, they build up in the cat’s body, and then have dangerous consequences making the cat extremely ill. The bladder often becomes hard and very painful for the cat as well.
How can I tell that my cat’s urethra may be obstructed?
It is important to realise that not all cats with urethral obstruction show the same signs. Some may just show non-specific signs such as being off their food or a little quieter than normal. Vomiting may occur, and at the opposite end of the spectrum some cats become very depressed and collapsed. There are some classical signs associated with urethral obstruction but remember that not all cats show these signs:
- Straining to urinate, maybe crying out when doing so
- Making frequent visits to the litter tray but only passing a few drops each time (‘spotting urine’)
- Discoloured urine due to blood
If your cat strains in the litter tray you should try and pay attention to whether they have passed faeces recently or not. Carers sometimes ring worried that their cat is constipated and then it turns out that in fact their bladder is blocked and the straining was because the cat is unable to pass urine.
Other signs that cats with urethral obstruction may show include:
- Walking abnormally at their back end – carers often mistakenly think the cat has had an accident of some sort
- Yowling as if in pain when picked up
It is essential to seek veterinary attention if you notice any of these signs in your cat, especially if the cat is male
by on February 3rd, 2014
Category: News, Tags:
The cornea, the outermost layer of the eye, is a very special tissue that is completely transparent. In contrast to the skin, it lacks pigment and even blood vessels to maintain its transparency. The cornea is very rich with nerves, making it a very sensitive tissue. This is the reason why even small particles such as dust on the surface of the eye can be so uncomfortable.
The cornea is made of three layers:
- a very thin outer layer (epithelium)
- the thick middle layer (stroma)
- a very thin inner layer (endothelium)
All three layers are important for the cornea to work. The outer layer or ‘epithelium’ can be thought of as a layer of cling film that forms the surface of the cornea and protects it from infections. It works as a shield to the eye. The thick middle layer or ‘stroma’ is what gives the cornea its strength and stability.
Corneal ulcers are classified by the depth, depending on the layers they affect. If only the epithelium is missing this is classified as a ‘superficial ulcer’ (or surface defect only). If the ulcer reaches into the stroma it is classified as a ‘deep ulcer’.
While superficial or surface ulcers are uncomfortable and present a risk of infection to the eye; the eye is not at the risk of bursting unless additional problems occur. However when the ulcer gets deep the eye becomes weak and can even perforate. Deep ulcers lead to visible indentations on the surface of the eye and can be accompanied by inflammation inside the eye.
Signs of corneal ulcers usually include eye pain (squinting, tearing, depressed behaviour) and ocular discharge, which can be watery or purulent.
Sometimes a lesion may already be visible on the surface of the eye. In this case it is particularly important to seek help from your veterinary surgeon as soon as possible.
How is a corneal ulcer diagnosed?
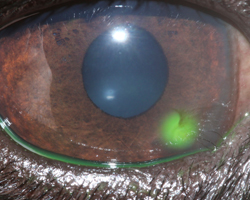
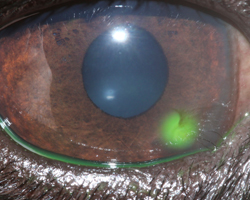
To diagnose a corneal ulcer your vet may use a special dye that highlights any defects of the surface layer by staining the underlying tissue green (See Photo). This test is called the fluorescein test.
Why do corneal ulcers occur?
When the presence of an ulcer has been confirmed, it is important to try and find a reason for it. Most ulcers occur due to an initial trauma. This is more likely to happen in dogs and cats with very prominent eyes (also called ‘brachycephalic’ animals), for example in Pugs and Pekingese dogs or Persian cats. In cats the flare up of a Feline Herpes Virus infection is also a common cause for the development of a corneal ulcer. Many conditions can increase the risk of corneal ulcers. Reduced tear production is a common contributing factor, but other conditions such as an incomplete blink, in-rolling of the eyelid (also called ‘entropion’) or eye lid tumours may contribute to the occurrence, but even more so may interfere with the healing process.
How are corneal ulcers treated?
To treat an ulcer it is essential that the underlying cause is identified and if possible corrected. This will stop the ulcer from getting worse and allow the eye to heal as quickly as possible. The treatment plan will usually include eye drops to treat or prevent infection but may include other medication depending on the cause and severity of the ulcer. Painkillers and/or antibitotics by mouth may also be necessary.
Do any corneal ulcers require an operation?
If an ulcer is deep or the cornea is even ruptured, surgery is required to save the eye. Different techniques are available, but all of them place healthy tissue into the defect to stabilise the cornea. Very small suture material, as thin as a human hair, is used to repair the cornea and an operating microscope should be used to handle the small and very fine structures of the eye. Grafting surgeries are very successful in saving eyes, but can lead to scaring of the cornea leaving it less transparent in areas.
How can corneal ulcers be prevented?
Corneal ulcers are best prevented and if they are present they should be treated as soon as possible to stop them from getting bigger and deeper.
Particularly in patients with prominent eyes, regular eye examinations should be performed to detect weaknesses in the corneal health. Indications of that may include white or brown marks on the surface of an otherwise comfortable eye or sticky discharge that continues to recur. Any painful eye should be presented to a veterinary surgeon as soon as possible.
Eyes may be cleaned with tap water that ideally should be boiled and cooled down again, using a lint-free towel. This should however not replace or delay the visit to a veterinary surgeon, as many ulcers require medication to achieve fast healing and prevent ill effects to the transparency of the cornea and therefore the sight of the dog or cat. Particularly; if a deep indentation or bulging tissue is noted on the surface, the eye should not be manipulated to prevent any additional damage.
 With November fast approaching now is the time to take appropriate steps to alleviate a potentially distressing time for your pet.
With November fast approaching now is the time to take appropriate steps to alleviate a potentially distressing time for your pet.
 The most unexpected things around the home and garden can present a hazard to your pets. This week we look at ten unexpected dangers you might not have been aware of. Prevention is better than cure – if you can, always ensure that potential hazards are kept securely away from your animals, and take what steps you can to prevent exposure. If you suspect your pet may have eaten or encountered any of the hazards discussed in this newsletter, contact your vets straight away for advice and appropriate treatment; do this even if your pet seems completely well, as with many of these dangers, there can be a delay of hours to days before signs of illness become apparent. Starting treatment before the pet starts to appear unwell can significantly improve the odds of them making a full recovery.
The most unexpected things around the home and garden can present a hazard to your pets. This week we look at ten unexpected dangers you might not have been aware of. Prevention is better than cure – if you can, always ensure that potential hazards are kept securely away from your animals, and take what steps you can to prevent exposure. If you suspect your pet may have eaten or encountered any of the hazards discussed in this newsletter, contact your vets straight away for advice and appropriate treatment; do this even if your pet seems completely well, as with many of these dangers, there can be a delay of hours to days before signs of illness become apparent. Starting treatment before the pet starts to appear unwell can significantly improve the odds of them making a full recovery. Many of us value our hens like our other family pets and want to be able to get professional advice and treatment if they fall ill. Currently most vets get minimal training on backyard chicken diagnosis and care, but with increasing numbers of hens now being kept across the country because of our re-homing initiative, there is a growing demand for specialist knowledge and treatment.
Many of us value our hens like our other family pets and want to be able to get professional advice and treatment if they fall ill. Currently most vets get minimal training on backyard chicken diagnosis and care, but with increasing numbers of hens now being kept across the country because of our re-homing initiative, there is a growing demand for specialist knowledge and treatment. Having trouble breathing is, at the very least, an uncomfortable experience, but can also be life-threatening if your pet is unable to take in enough oxygen to their lungs when breathing in, or to get rid of enough carbon dioxide from their lungs when breathing out.
Having trouble breathing is, at the very least, an uncomfortable experience, but can also be life-threatening if your pet is unable to take in enough oxygen to their lungs when breathing in, or to get rid of enough carbon dioxide from their lungs when breathing out. Last year only half of the UK dog and cat population were fully protected against infectious diseases. Was your pet one of them?
Last year only half of the UK dog and cat population were fully protected against infectious diseases. Was your pet one of them? Ticks are second only to mosquitoes throughout the world in transmitting infectious disease to humans and animals.
Ticks are second only to mosquitoes throughout the world in transmitting infectious disease to humans and animals.