News
Addison’s Disease (Hypoadrenocorticism)
by admin on January 3rd, 2020
Category: News, Tags:
What is Addison’s Disease?
Addison’s Disease is also called ‘hypoadrenocorticism’. This is a potentially life-threatening disorder caused by inadequate levels of hormones produced by small glands which are located in the abdomen (the tummy) near the kidneys. The adrenal glands produce two types of hormone that are critical for life:
- Glucocorticoids
- Mineralocorticoids
These hormones circulate through the blood stream and have effects on cells and tissues throughout the body. Dogs or cats with insufficient levels of these hormones can become very unwell.
Glucocorticoids are a natural form of cortisone (steroid). Cortisone is essential for life and must be at the right levels in the body for animals (and humans) to feel well. Steroids improve appetite and have effects on the function of the immune system that fights off infections.
Glucocorticoids can also be used as a drug for the treatment of some diseases.
Too little natural circulating cortisone is one of the components of Addison’s Disease (too much circulating glucocorticoid also causes a problem called Cushing’s Syndrome). Mineralocorticoids are also hormones produced by the adrenal glands.
Mineralocorticoids help to control the body’s ‘salt’ concentrations of both sodium and potassium. As with glucocorticoids, too much or too little mineralocorticoid in the body generally results in serious medical problems.
Addison’s Disease occurs when the body has insufficient circulating levels of both glucocorticoids and mineralocorticoids.
What causes Addison’s Disease?
Addison’s Disease results when both of the adrenal glands are damaged. This most commonly occurs when the affected animal’s own immune system, which normally fights off infections, becomes overactive and damages the adrenal glands (so called ‘immune mediated’ disease). Less common causes of Addison’s Disease are cancers or infections that can invade and kill the adrenal gland tissues.
Which animals are predisposed to Addison’s Disease?
Although Addison’s Disease is not very common, it occurs most frequently in young to middle-aged female dogs. Addison’s Disease is considered rare in cats, but the condition has been diagnosed in dogs and cats of all ages and of either sex (including neutered animals of both sexes).
Breeds that appear to be predisposed to Addison’s Disease include Portuguese Water Dogs, Standard Poodles and Bearded Collies, although it can affect any breed and crossbred dogs.
What are the symptoms (signs) of Addison’s Disease?
The signs of Addison’s Disease come on quickly, usually over a few days, although they can also appear over a period of months. Most owners notice that their pet develops several problems at about the same time including;
- Reduced appetite
- Lethargy and weakness
- Vomiting
- Diarrhoea
- Weight loss
- Tremors
In severe cases some dogs will suddenly collapse and develop shock-like symptoms.
What tests are needed to diagnose Addison’s Disease?
The signs of vomiting, diarrhoea, loss of appetite, and weight loss are extremely non-specific – many other conditions such as stomach and intestinal disease, kidney disease and pancreatic disease can cause these symptoms. Further tests are therefore needed to determine the cause of these problems.
Changes that may be noted on blood tests include changes in the salt levels in the blood – an increase in potassium and a decrease in sodium are major findings. However, these changes can also be seen with other disease processes, and if Addison’s Disease is suspected, a specific test is then recommended for confirming the diagnosis – this is called an ‘ACTH stimulation test’.
What treatment is needed if Addison’s Disease is diagnosed?
Initially, most patients with Addison’s Disease have severe dehydration and electrolyte (salt) loss, meaning that they need to be hospitalised for initial treatment and stabilisation.
Once stabilised, patients with Addison’s Disease require long term (lifelong) treatment with hormone replacement, to substitute for the missing mineralocorticoids and glucocorticoids. These drugs can be given at home in the form of tablets or injections.
The amount of medication may need to be changed over time, and frequent blood tests are recommended to monitor the condition and improve the chances of good control of the disease.
If dogs are stressed (for example due to going to boarding kennels, or because of other illness) your vet may guide you to administer some additional steroid therapy.
What’s the prognosis (outlook)?
Once dogs and cats with Addison’s Disease are correctly diagnosed and properly treated, they can live long and happy lives. Treatment is almost always successful and rewarding.
Pet of the month – January 2020
by admin on January 3rd, 2020
Category: Pet of the Month, Tags:
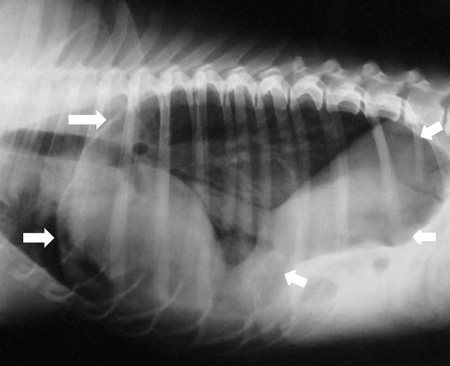
Pet of the month for January is Red who is a registered Hearing Dog. Unfortunately on a recent walk he found something appealing to devour that came with a fish hook attached.
Red is seen here post surgery to remove the hook that was found on radiography to be located in his stomach. We are delgihted to report that he is recovering very well.
Chronic liver failure
by admin on December 2nd, 2019
Category: News, Tags:
The liver is a vital organ – animals and people cannot survive without their livers. The liver performs many complex functions that are essential to life and good health. Its main functions are:
- To convert food into useful substances such as proteins for repair and growth of the body
- To maintain normal functions such as blood clotting, fighting infection and secretion of substances to the bloodstream
- Bile production, which assists with the absorption of fat and certain vitamins
- To store the body’s primary sugar (glucose) as glycogen and be able to release it into the bloodstream when it is needed
- To neutralise and break down toxic substances such as chemicals and some medications, for later elimination in bile or through the kidneys
What is chronic liver failure?
Chronic liver failure occurs due to long-term damage to the liver, resulting in a liver that fails to work. Chronic liver failure can be caused by chronic exposure to toxins, heavy metals (copper, iron and zinc), chronic infections, chronic inflammation/irritation, cancer, blood vessel abnormalities (congenital portosystemic shunt – an abnormal blood vessel that a pet is born with that bypasses the liver), immune disease and fatty liver syndrome in cats.
The liver is very good at regenerating itself (unlike other organs such as the kidneys), but serious ongoing damage to the liver can cause long-term failure of its function – this is known as chronic liver failure. Over 75% of the liver is usually damaged before liver failure occurs.
What are the signs of chronic liver failure?
- Reduced appetite
- Lethargy
- Increased thirst
- Strange behaviours
- Vomiting
- Diarrhoea – occasionally blood in the stools, or dark, tarry stools
- Bloated tummy due to fluid accumulation
- Yellow skin, urine, gums (jaundice)
- Weight loss
How is chronic liver failure diagnosed?
Liver failure is diagnosed by blood tests which indicate dysfunction of the liver. Further investigations, such as ultrasound scans, urine cultures, blood cultures or other tests for infections, may be required in individual cases. Samples of the liver may be required to diagnose the cause of liver failure in many cases – these may be obtained through a needle placed in the liver under guidance on an ultrasound scan; alternatively the liver may be visualised by using keyhole surgery (laparoscopy) or by a full surgical procedure. The technique that is chosen will depend on a number of factors, and these will be discussed with you in the event that biopsies are required. In some cases of chronic liver disease the initial cause of the problem may no longer be present at the time of investigation, but the disease itself may still cause symptoms, and the damage to the liver may also continue.
How is chronic liver failure treated?
Chronic liver failure requires multiple treatments. It is important to try to remove the initiating cause (e.g. toxins, infections, cancer etc). Sometimes, this is not possible and it is best to support liver function and make the patient as comfortable as possible. Some diseases e.g. blood vessel abnormalities such as congenital portosystemic shunts (abnormal blood vessels that bypass the liver) can be corrected by Specialist surgical procedures.
Treatments which may be required in chronic liver failure include:
- removing fluid from the abdomen that accumulates due to scarring of the liver
- antibiotics to prevent infections
- antacids to reduce gastrointestinal ulceration
- drugs to support the liver including anti-oxidants, anti-
scarring drugs and drugs that bind to heavy metals i.e. copper and zinc - dietary modification to reduce protein and copper levels in some patients
- nutritional support – an adequate intake of vital nutrients including calories is very important in cases of chronic liver failure.
What is the long term outlook?
Considering the severity of this disease process, this is a challenging condition to treat. Early intervention and aggressive treatment can be successful in some cases where the extent of damage is not too severe. At the present time, liver transplants are not available in veterinary medicine.
If your pet develops chronic liver failure, we will discuss the treatment options in detail with you and give you the help you need in making decisions about what you wish us to do to help your pet.
Pet of the month – December 2019
by admin on December 2nd, 2019
Category: Pet of the Month, Tags:
Henry had been struggling with his weight and came to see our weight management nurse Sienna. She has helped his owners devise a feeding plan and weight loss plan to ensure he has a steady and easily maintainable weight loss. Being a British Bulldog it is very important for him to be as slim as possible to optimise his breathing and there are many other associated health benefits for this breed. Henry has made great progress and can even jump up on the furniture now as seen in the accompanying picture.
If you would like more information on Sienna’s weight clinics then please call us, we’d be happy to help!
Hiatal Hernia
by admin on November 5th, 2019
Category: News, Tags:
What is a Hiatal Hernia?
A hiatal hernia is the abnormal movement of part of the stomach from its normal position in the abdomen into the chest.
The diaphragm is a sheet of muscle which separates the chest and abdomen. The oesophagus (food pipe) and major blood vessels and nerves pass through the diaphragm via small openings within the muscle. During the development of a puppy, these openings may be excessively large, allowing organs which should remain in the abdomen to pass into the chest. The stomach can become permanently displaced but more commonly slides back and forth between the abdomen and the chest.
What breeds are affected?
English Bulldogs are the breed most commonly seen with this condition in the UK. Brachycephalic dogs (those with a shortened nose such as English Bulldogs, French Bulldogs and Pugs) are at an increased risk of displacement of the stomach into the chest as the negative pressures within the chest created by their abnormal airway, act to ‘suck’ the stomach through the opening in the diaphragm.
What are the symptoms?
Dogs with hiatal hernia frequently vomit or regurgitate (passive reflux of stomach contents) due to the abnormal position of the stomach. These signs most commonly occur during peak exercise or when the dog becomes excited. Reflux of acidic stomach contents into the oesophagus results in inflammation (reflux oesophagitis) which can trigger a self-perpetuating cycle of regurgitation causing further inflammation.
Other symptoms which may be observed include excessive salivation, poor appetite and weight loss. Vomiting and/or regurgitation of stomach contents can result in inhalation of this material and the development of secondary pneumonia. In this scenario symptoms such as a cough, nasal discharge and breathing difficulties will be observed.
How is the diagnosis made?
Hiatal hernia is most commonly diagnosed via fluoroscopy (a moving x-ray study). Whilst the dog is eating, a continuous run of X-rays are taken which allows the swallowing process and position of the stomach to be closely observed. Typical findings consistent with a diagnosis of hiatal hernia are food entering the stomach and then passing back up the oesophagus (reflux) along with movement of the stomach back and forth across the diaphragm.
As the stomach typically slides back and forth from a normal to abnormal position, there is the possibility that the imaging study documents a normal stomach position. This does not exclude the diagnosis of hiatal hernia as the most likely explanation for a normal stomach position is that the stomach has not been ‘captured’ in an abnormal position at the time of the imaging study. If this scenario arises, a presumptive diagnosis of hiatal hernia may be made based on the breed of the dog and the symptoms.
What treatment options are available?
The management of hiatal hernia can be broadly divided into medical and surgical options.
Medical management consists of the use of medication to reduce inflammation within the oesophagus (antacids) and aid motility of the gastrointestinal tract. Medication often reduces the severity and frequency of the symptoms but is unlikely to eliminate them completely due to the persistently abnormal position of the stomach.
Surgical correction is often indicated to resolve the clinical problems. In some patients surgical correction of the upper airway problems, as seen in Brachycephalic dogs, eliminates the problems. In other patients the surgery will consist of reducing the size of the overly large opening in the diaphragm and stitching the oesophagus and stomach permanently in a normal position. This technique prevents movement of the stomach into the chest.
What is the outlook (prognosis) for my dog?
The prognosis following surgery is good. The aim is to eliminate the symptoms (regurgitation and vomiting) completely. Rarely, dogs may continue to regurgitate and/or vomit after surgery although with a markedly reduced frequency compared to before surgery. If this is the case, these mild symptoms can usually be controlled with the use of medication.
Pet of the month – November 2019
by admin on November 5th, 2019
Category: Pet of the Month, Tags:
On previous occasions, in addition to socks, Hubble has swallowed a tea towel and a stone.
Let’s hope this is the last time!
Canine Flank Alopecia
by admin on October 1st, 2019
Category: News, Tags:
What is canine flank alopecia?
Canine flank alopecia is a localised, often cyclic, disease of the hair follicles resulting in hair loss over the flanks of affected dogs. It is also known by the names cyclic flank alopecia, recurrent flank alopecia and seasonal flank alopecia, but these terms are not always accurate as the condition can appear at various times of the year, vary in duration, be continuous or be sporadic in nature.
What causes flank alopecia?
The cause of this condition is not known. However, as hair loss often occurs at times of the year when day length is at its shortest, light exposure may be involved. The mechanisms by which this might occur are not understood at present.
What are the clinical signs?
Canine flank alopecia occurs in dogs with ages ranging from 1 year to 11 years, although most cases develop between 3 and 6 years. This condition is seen more commonly in breeds such as Boxers, Airedale terriers, English Bulldogs and Schnauzers.
The condition causes areas of non-itchy hair loss over the flanks of affected dogs (Figure 1). The skin at the affected sites usually appears normal, although it often becomes very dark with pigmentation, and hair re-growth of a different colour sometimes occurs. Surrounding hair and skin is usually normal. Canine flank alopecia can occur on both sides of the dog or be limited to one side, and hair loss can also occur over the base of the back (Figure 2). The disease in some dogs is cyclic, with hair loss occurring at the same time each year and hair re-growth occurring in the times between. In other dogs, hair loss is more permanent, and no re-growth is seen following the initial loss. Some dogs are reported as only having one cycle of hair loss and re-growth in their lives.
How is it diagnosed?
The diagnosis of canine flank alopecia can often be made based on the clinical findings, since the lesions are so striking. Some hormonal diseases of dogs can present with non-itchy hair loss, so blood and urine tests may be warranted if there is a concern about these diseases.
Additionally, biopsies of affected skin can be taken which are then sent off for analysis at a laboratory. Biopsies can be supportive of a diagnosis of canine flank alopecia.
What are the treatments available?
Canine flank alopecia is a cosmetic disease. As dogs remain healthy, with many re-growing their hair eventually, a decision not to treat the affected dog is often taken.
If treatment is requested, melatonin is generally considered the treatment of choice as it is relatively safe and inexpensive. It is difficult to judge the response to medication though due to the high rate of spontaneous hair re-growth.
What is the outlook/prognosis?
The prognosis for this cosmetic disease is good, with dogs remaining systemically healthy despite unpredictable hair growth. The prognosis for full and normal hair re-growth at affected sites is also often good, but the disease is highly variable.