News
Hyperthyroidism in Cats
by admin on September 1st, 2016
Category: News, Tags:
What is hyperthyroidism?
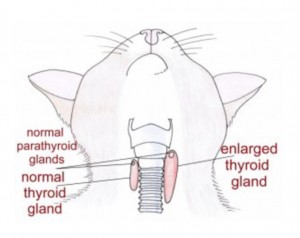
Hyperthyroidism is a relatively common disease of the ageing cat. It is typically the result of a benign (non-cancerous) increase in the number of cells in one or both of the thyroid glands. The thyroid glands are located in the neck although there is occasionally additional tissue within the chest. In the image the red shapes indicate approximately where the thyroid glands are located in a cat. The result of enlargement of the thyroid glands is an increased production of thyroid hormone within the body. Thyroid hormone controls the rate at which cells in the body work; if there is too much hormone, the cells work too fast. Despite many years of research the exact cause of hyperthyroidism remains unknown.
Cats fed almost entirely canned food have been reported to have an increased risk of developing hyperthyroidism but it is likely that there are many causes.
What signs do cats with hyperthyroidism get?
Hyperthyroidism is a disease of middle aged to older cats with an average age of onset of 12-13 years. Increased drinking and increased urination, weight loss, increased activity, vomiting, diarrhoea and increased appetite are often reported. Physical examination often reveals a small lump in the neck which represents an enlarged thyroid gland.
How is hyperthyroidism diagnosed?
A diagnosis of hyperthyroidism is made by the demonstration of increased levels of thyroid hormone in the blood stream. Thyroxine (T4) measurement is the initial diagnostic test of choice.
How is hyperthyroidism in cats managed?
- Medical treatment with either carbimazole or methimazole. These tablet medications are given once or twice daily lifelong. Side effects are uncommon but can occur. They include vomiting and reduced appetite. Very occasionally severe bone marrow or liver problems can be seen.
- Dietary treatment. A specific prescription diet can be fed to hyperthyroid cats to control the disease. The diet is very low in iodine. Iodine is an essential component of thyroid hormone and less dietary iodine means less thyroid hormone is produced. The diet must be fed exclusively (i.e. the cat must eat no other food). Dietary treatment does not lower the thyroid hormone levels as much as the other treatment options
- Surgical treatment. One or preferably both thyroid glands are removed with an operation. A short period of treatment with tablets is recommended prior to surgery. Anaesthesia can be a risk in older cats with hyperthyroidism that possibly have other concurrent diseases. There is a risk of a low blood calcium level after surgery if the parathyroid glands are removed with the thyroid glands. This can be a very serious problem if it is not recognised. Signs of a low blood calcium level can include facial rubbing, fits, tiredness, reduced appetite and wobbliness. Low blood calcium levels are relatively easily managed with oral medication and treatment is rarely necessary lifelong.
- Radioactive iodine treatment. Radioactive iodine is concentrated in the thyroid gland and destroys excessive thyroid tissue. The drug is given by injection under the skin. After the injection, cats need to spend 2-4 weeks in an isolation facility whilst they eliminate the radioactive material. Owners are not able to visit their pets whilst they are in isolation.
- Hyperthyroidism can mask underlying kidney problems and these can become apparent after treatment. Blood tests will be necessary to assess kidney function as well as the thyroxine level during/after treatment.
Can dogs get hyperthyroidism?
Dogs are rarely affected by hyperthyroidism and when it occurs in this species it is normally the result of a diet problem or cancer of the thyroid gland. Treatment for dogs with cancer of the thyroid gland can involve one or a combination of surgery, radioactive iodine, radiation therapy and chemotherapy. Unfortunately many dogs have advanced disease by the time the cancer is identified. The majority of dogs with thyroid cancer are not hyperthyroid; they typically retain normal thyroid function or become hypothyroid.
Responses are currently closed, but you can trackback from your own site.