News
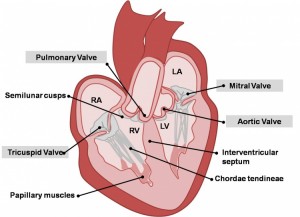
What is a Heart Murmur?
by admin on March 10th, 2021
Category: News, Tags:
- Murmurs explained
- FAQs about murmurs
- List of the common causes of murmurs in dogs and cats
- Murmurs explained
- FAQs about murmurs
- List of the common causes of murmurs in dogs and cats
- Mitral Valve Disease (MVD) is the most common cause of a murmur in adult dogs in older age
- Mitral Valve Dysplasia is a congenital defect of the valve
- Mitral Valve Regurgitation can occur secondary to heart enlargement of other causes in dogs
- Mitral Valve Regurgitation can be secondary to cardiomyopathy in cats
- Subaortic Stenosis and Valvular Aortic Stenosis is a congenital defect of the valve
- Hypertrophic Cardiomyopathy in cats, often causes ‘Subaortic- like Stenosis’
- Tricuspid Valve Disease occurs in adult dogs in older age, most will also have MVD
- Tricuspid Valve Dysplasia is a congenital defect of the valve
- Tricuspid Valve Regurgitation can occur secondary to Pulmonary Hypertension
- Tricuspid Valve Regurgitation can be secondary to heart enlargement of other causes
- Tricuspid Valve Regurgitation, when mild, can be seen in some normal dogs
- Valvular Pulmonic Stenosis is a congenital defect of the valve
Murmurs associated with holes in the heart
- Patent Ductus Arteriosus is a congenital defect resulting in abnormal flow between the aorta and pulmonary artery
- Ventricular Septal Defect is a congenital defect in which there is a hole between the two ventricles
- Puppy murmurs are innocent murmurs that usually disappear by 4-6 months of age
- Anaemic murmurs are due to the blood being thin
- Fever murmurs are due to turbulence in blood flow
- Flow murmurs are seen in some athletically fit dogs, ie. a murmur with no defect present
Pet of the month – March 2021
by admin on March 10th, 2021
Category: Pet of the Month, Tags:
Pet of the month – July 2020
by admin on July 7th, 2020
Category: Pet of the Month, Tags:
Meet Wilson. In the Spring he became intermittently lame on his right back leg. Anti-inflammatory medication helped but did not resolve the lameness so we x-rayed his leg.
Imagine the shock when it was discovered that Wilson had a shotgun pellet embedded deeply in his leg which had caused a non-displaced spiral fracture of his femur. A specialist was consulted but fortunately Wilson only required cage rest for 4 weeks and it was decided that it was best to leave the pellet in situ unless infection developed.
We are delighted to say that Wilson has made a full recovery.
COVID-19 UPDATES
by admin on July 7th, 2020
Category: News, Tags:
We are pleased to report that our Littlehampton Clinic is open and we have resumed services with social distancing measures in place.
We are allowing our two legged friends into the practice with their pets but our passageways and consulting rooms are narrow so in order to maintain social distancing we ask that you notify us when you have arrived, by phone or tapping on the window, and remain outside until invited to enter, to avoid crowding.
Hand hygiene stations have been installed on entry to the main building and at reception, as well as screens at reception.
Please respect our social distancing measures which will include asking that only one owner accompanies per pet, and highlight that our preferred payment method is by card. We request face coverings and you may be asked to wait outside if you do not have one.
In the consulting room we will ask you to remain seated whilst a vet and nurse examine your pet.
We request that wherever possible repeat medications are paid for in advance over the phone by card, so that interaction is kept minimal on collection.
Due to the ways of working we have had to adopt to keep our staff, you and your pets safe, things are taking us a bit longer, reducing the number of pets we can see in practice every day. Please bear with us while we continue to prioritise in-practice appointments and operations, and offer video or telephone consults for some pets.
We hope to re-open our branches in due course. Social distancing requirements mean that for the time being our clients may not hold their pets during examination. We are therefore having to recruit a nurse to assist in this capacity and will probably need to introduce appointments to avoid crowding when we re-open in Arundel and Angmering.
We would like to say a massive THANK YOU to all our customers for being so understanding and accommodating at this difficult time.
Pet of the month – June 2020
by admin on June 16th, 2020
Category: Pet of the Month, Tags:
Bob is one of many cats we care for who suffers from IBD (Inflammatory Bowel Disease).
IBD is not a single disease but a group of chronic gastrointestinal disorders caused by an infiltration of inflammatory cells into the walls of a cat’s gastrointestinal tract. The infiltration of cells thickens the wall of the gastrointestinal tract and disrupts the intestine’s ability to function properly. IBD occurs most often in middle-aged and older cats.
What does the future hold for a cat with IBD?
IBD is a chronic disease. Few cats are actually cured, and symptoms may wax and wane over time. IBD can often be controlled such that affected cats are healthy and comfortable. Vigilant monitoring by the veterinarian and owner is critical.
We are very pleased to report that Bob has responded well to dietary management and is currently not requiring additional medication. Luckily he is not adept at hunting and so we have no fear that he might cause a flare up through illicit snacks!
Covid-19 Update & Out of Hours Provision
by admin on June 16th, 2020
Category: News, Tags:
Transitioning to a more normal range of veterinary services:
In line with the easing of restrictions across the UK, our governing body are allowing us to begin transitioning towards providing as full a range of veterinary services as possible in a safe manner. However, during the pandemic it will not be a return to pre-Covid ‘business as usual’. We will be increasing our services this week by degrees, and in relation to demand.
Safe working:
All our services have to be risk assessed and provided in a manner that supports safe working and recognises 2m Social Distancing. Our premises do not lend themselves to the necessary social spacing that is possible in supermarkets and high-street stores, nor do our consulting rooms.
Visiting the clinic:
Creating a socially-distanced queueing system in our limited space would seriously delay pets arriving for urgent appointments so we respectfully request that all clients arriving at the clinic do not enter but instead:
- Call us, confirm their mobile phone number, and supply their car type and registration if applicable
- Clients without mobile phones, please knock on the window
- Please be prepared to remain outside the clinic e.g. in a car
Pets will be collected from holding zones and examined. The vet will then contact you and treatment plans will be agreed remotely. Payment can be made over the phone.
Contact-free collection of medication, pet food and anti-parasitic medications is in place and a specific, secure collection time and place can be organised in advance. For any products you’d like to order simply call us to arrange for payment and safe collection of these items.
Where appropriate you will be offered video or telephone consults, enabling you to get the advice you need and for our team to decide if we need to see your pet in person to provide further care. For any emergencies or seriously ill pets we will ask you to attend the practice.
Your safety and the safety of our teams is our top priority so please follow the social distancing procedures we have in place to minimise contact.
We apologise that formerly simple procedures and transactions are taking much longer than was usual, for reasons of social distancing. Your co-operation and patience are greatly appreciated.
Out of Hours Services:
From Monday 15th June our out of hours emergencies will be attended by Worthing Emergency Vets based at Grove Lodge Veterinary Hospital in Worthing, West Sussex, for a trial period of 3 months. Please rest assured that all pets in our hospital will continue to be attended by one of our vets and nurses outside opening hours, and will not be transferred to Worthing.
At the end of March two of our team of vets departed for new positions but were not replaced because of lockdown. The remaining small team of vets continued to provide emergency cover. We are sad to say that this reduced team are no longer able to continue to provide 24 cover whilst at the same time returning to normal working hours, and the volume of work the clinic is currently allowed to undertake does not allow for replacement of these team members at present.
COVID-19 Update & article on Feline Lower Urinary Tract Disease
by admin on May 5th, 2020
Category: News, Tags:
Our main Littlehampton hospital REMAINS OPEN and in line with government guidelines small teams are working 24-hour shifts to provide emergency care and urgent treatment where animal welfare would be compromised by delay, as well as providing repeat medicines.
Concerned about your pet’s health but don’t think it’s an emergency?
If you are worried about your pet, please phone us and explain your situation. We’ll arrange a suitable way of conducting your appointment that is in everyone’s best interests.
There are a variety of options available to everyone – the important thing is to let us know and we’ll work together!
To respect social distancing rules, we are replacing our standard consultation service with video and telephone consultations. Please contact the practice to arrange an appointment and discuss suitable communication platforms (eg Skype, Facetime, WhatsApp). Payment can be made over the phone.
What constitutes an emergency that needs immediate care?
If any of the below apply to your pet, contact us IMMEDIATELY:
- Breathing difficulties
- Open wound injuries
- Trauma (e.g. car accidents)
- Male cats struggling in the litter tray to pass urine
- Rabbits neglecting food
- Swallowing hazards ie.toys/clothes
- Ingestion of poisonous/harmful substances
- Eye problems
- Vomiting or diarrhoea especially if your pet appears quiet or depressed or if it is going on for a long time (more than 24 hours)
- Swollen abdomen or retching (especially large dogs)
- Loss of thirst & appetite
- Struggling to give birth
- Seizuring/fitting
- Collapse
If the recommendation is to come into the practice, please note the following advice to keep you and our staff safe:
- We will ask that you telephone us when you arrive in the car park.
- A member of staff will come out and take your pet into the clinic.
- After making an assessment we will ring you on your mobile to discuss the necessary treatment and way forward.
Can I bring my pet in for an INITIAL VACCINATION COURSE?
Unvaccinated puppies, kittens and rabbits are at risk from picking up the diseases we commonly vaccinate against.
Whilst the risk can be lessened by keeping pets inside and avoiding contact with unvaccinated animals, please contact us to discuss your pet’s current situation with you, and risk assess whether vaccination at this point is recommended.
Can I bring my pet in for their ANNUAL VACCINATION BOOSTER?
We can postpone this vaccine for up to 3 months after the due date without requiring a restart. During these exceptional times, we ask that you delay the booster, but for no more than a maximum of 3 months after the due date.
Can I bring in my pet for a HEALTH CHECK?
Not at this moment in time because this is not deemed critical. However, if your pet is ill we will be able to conduct a consultation via a video or telephone consultation. Please ask the practice for further information.
Can I bring my pet in for NAIL CLIPS? Or to have their ANAL GLANDS expressed?
This should be postponed, provided your pet is not suffering pain or discomfort.
How can I get my REPEAT FOOD or MEDICATIONS?
It is important that you continue to give your pet the appropriate food and medication. We are looking at ways of getting these to clients who are due them and postal / delivery services may be an option. Please contact us to make suitable arrangements.
How can I get my FLEA, WORM, TICK and FLYSTRIKE treatments?
It is important that you continue to give your pet the appropriate treatments. We are looking at ways of getting these to clients who are due them and postal / delivery services may be an option. Please contact us to make suitable arrangements.
Can my pet still have ELECTIVE OPERATIONS such as Neutering and Lumps removals?
These operations are not deemed to be critical during these extraordinary times and we therefore ask that unless your pet’s health is being endangered, you postpone these procedures until government guidelines on social distancing change. If you have specific concerns please contact us to discuss your pet’s current situation, and risk assess whether surgery at this point is recommended.
What about ULTRASOUNDS and BLOOD TESTS?
It depends whether these are deemed critical or not – please contact us to discuss.
Please continue taking care of yourselves and all your lovely pets!!
WHAT IS FLUTD?
FLUTD stands for feline lower urinary tract disease. This is a term used to describe a collection of conditions which can affect the bladder and/or urethra (tube from the bladder to the outside).
The most common conditions causing FLUTD are:
- Urolithiasis (stones in the bladder and/or urethra)- there are various different stones which can form in the urinary tract resulting in FLUTD due to irritation of the bladder/urethral lining.
- Structural defects- rarely some cats can be born with anatomical defects which can lead to signs of FLUTD. Alternatively a defect such as a stricture (narrowing of the urethra secondary to scar formation) can develop in older animals.
- Bacterial infection- this is a relatively uncommon cause of FLUTD. In some cases an infection can be present alongside another condition.
- Cancer- tumours of the bladder and/or urethra are thankfully rare in cats.
- Urethral plugs and urethral spasm- urethral plugs are accumulations of cells, cyrstals and other debris which, if formed in the urethra, can block urine output from the bladder in male cats. In addition spasm (muscular contraction and narrowing) of the urethra can occur which can also result in blockage of the urethra.
- Feline Idiopathic Cystitis (termed F.I.C.)- this is the most common cause of FLUTD (around 60-70% of cases). The exact cause of F.I.C. is unknown although there are studies which suggest that this condition results from an abnormal response to stress. This condition is diagnosed after excluding all other causes however many cats with other conditions (for example urethral plugs/spasm) will also have F.I.C.
What are the signs of FLUTD?
The most common clinical signs of FLUTD relate to abnormalities of urination. In some cats which only urinate outdoors signs may not be apparent at home. If observed signs would include:
- Straining to urinate
- Crying when urinating
- Urinating in inappropriate places
- Urinating more often than normal
- Smaller volumes of urine produced when urinating
- Inability to urinate (this can be life threatening, requiring immediate veterinary attention).
- Blood visible in the urine
- Over-grooming the perineum
- Signs of pain/inappropriate aggression particularly around the hind end.
How is FLUTD investigated?
Initially a thorough history including identification of any potential factors that could lead to stress (i.e. house move, new pet in the environment or building work at home) is taken. A physical examination will then be performed. In male cats the bladder size and texture will carefully be assessed to identify whether urethral blockage (obstruction) is present. Next a combination of some or all of the following tests may be performed:
- Urinalysis: This may be collected at home (free-catch) or by taking a sample directly from the bladder using a needle. The urine concentration is assessed alongside checking for bacteria, blood, protein or crystals.
- Blood tests: A blood sample may be taken, especially in cats with suspected urethral blockage. This is to assess kidney function and blood salt (electrolyte) concentration. In addition some cats can have alterations in blood calcium levels which could predispose to stone formation.
- Abdominal ultrasound: This can be used to check for any signs of a tumour or stones in the bladder. The bladder wall thickness can also be assessed.
- X-rays: Some bladder or urethral stones (uroliths) can be visible on an X-ray of the abdomen.
How is FLUTD treated?
The treatment of FLUTD will vary depending on the underlying cause. In general FLUTD is a painful condition and therefore in all cases pain relief is normally administered. A short summary of possible treatments for each cause is given below.
Urolithiasis
If bladder stones are causing clinical signs they may need to be removed. Some types of stones (e.g. struvite) can be dissolved by changing to a specifically manufactured prescription diet. Others are normally removed surgically. If a urethral stone is present and causing blockage then additional, emergency treatment is required. This is discussed in more detail in the “Urethral plugs and urethral spasm” section.
Structural defects
Often surgery is required to correct structural defects. In cats with urethral strictures, dependent on the location, a procedure called perineal urethrostomy can be performed to open the urethra above the narrowing, creating a permanent new location for urine to exit.
Bacterial infection
Bacterial infections are treated with antibiotics. Due to the increasing prevalence of resistance, antibiotics should only be used in cats where there is either a very strong suspicion of infection or confirmed infection (particularly as this is less common).
Cancer
The most common type of cancer found in the bladder is called transitional cell carcinoma. This is generally treated with a combination of chemotherapy and non-steroidal anti-inflammatories. Other benign tumours may be treated by surgical removal.
Urethral plugs and urethral spasm
Urethral plugs or spasm resulting in blockage of the urethra (normally in male cats due to the diameter, shape and length of the urethra) can be life threatening. This is because if it is left untreated the kidneys can become damaged and blood salts can become deranged leading to heart problems and even death.
Cats with urethral blockage are rapidly assessed. Normally pain relief and muscle relaxants are administered alongside fluid therapy into the vein. The patient is then either anaesthetised or heavily sedated and removal of the blockage is performed (normally by flushing and placement of a catheter through the urethra into the bladder). After the catheter is passed into the bladder it is often secured in place for a few days. This is prevent immediate re-blockage and to allow time for the spasm and associated inflammation/swelling of the urethra to improve. The catheter is then removed and the patients are observed to ensure that they are able to urinate.
In cats with kidney problems due to the blockage fluid therapy into the vein will need to be continued until the kidneys improve. Sadly in some cases permanent damage to the kidneys can occur resulting in chronic kidney failure. Thankfully this is uncommon.
Rarely it is not possible to unblock the urethra with a catheter. In addition some cats have recurrent episodes of urethral blockage despite preventative therapy. In this specific but small group of patients a perineal urethrostomy can be performed (as discussed in structural defects). It is important to understand that there can be serious complications associated with the surgery and it does cure the condition.
Feline Idiopathic Cystitis (F.I.C.)
The management of F.I.C. is complex as the cause is multifactorial. Factors thought to contribute to the condition include a defective bladder lining, stress (specifically an individual’s inappropriate reaction to stress) and inflammation caused by the central nervous system. In humans a similar condition exists called ‘interstitial cystitis’. Changes in the bladder lining and brain of cats with F.I.C. are similar to those found in humans with this disease.
There are various different treatments available, with evidence behind each recommendation varying in quality and quantity. A short summary of each therapy area is given below:
- Dietary medication: Simply changing from dry to wet (sachet or tinned) food can help to increase the amount of water consumed. This can result in the production of more dilute urine. There are various prescription urinary diets available which may be recommended in specific circumstances (particularly if struvite stones are present or high blood calcium).
- Increasing water intake: In addition to changing to wet food, cats with F.I.C. should be encouraged to drink more water to enhance the production of dilute urine. This can be achieved by providing a water fountain, ensuring fresh water is always available in multiple locations or adding water to food.
- Litter tray number and location: There should be at least one litter tray for each cat in the household. These should be placed in different locations, preferably in less busy areas of the home. The type of litter can also have an impact and therefore providing a few different types to evaluate which is preferred can help. Cats that normally urinate outside should not be forced to use a litter tray.
- Identification and modification of stressful stimuli: This is a very important part of management but is often the most difficult to practically achieve. If an event that would be anticipated to cause stress is to occur (i.e. house move or new pet) then measures to minimise the impact should be considered. It is thought that conflict with another cat in the same household is the most common cause of stress in cats with F.I.C. Signs of this may not be immediately obvious and resolving or improving this can be difficult. Encouraging play and the addition of new toys to the environment can help. In cats that are indoors only, allowing some outdoor access can help (if safely possible). Consultation with a behaviourist can also be required to identify and improve causes of stress.
- Painkillers: Chronic or intermittent pain relief can be prescribed. There are various types available including non-steroidal anti-inflammatories and opiods.
- GAG replacers: GAG replacers theoretically help cats with F.I.C. by improving the abnormal bladder lining. There are multiple different formulations available and some are present in prescription diets targeted for urinary tract disease.
- Synthetic pheromone therapy: Feliway® is a feline synthetic pheromone which may help to reduce stress and anxiety. There are various ways this can be used (either a spray or a plug-in diffuser). Further advice is available from the website and there are different products available to use in different scenarios (i.e. in multi-cat homes or during times of anticipated stress).
- Anti-depressants: In extreme cases human anti-depressants can be used. These are normally reserved for severely affected cats that are refractory to all other forms of therapy.
Pet of the month – May 2020
by admin on May 5th, 2020
Category: Pet of the Month, Tags:
Pet of the Month for May is handsome Hadley, who has featured in this slot before.
He rejoins us this month as a reminder of how short a time it takes for a pet to rifle through an owner’s bag when their back is turned – in this case eating a packet of ibuprofen!
Ibuprofen is highly toxic and will cause gastrointestinal upset, including ulceration and acute kidney injury.
Luckily Hadley’s predilection for items that cannot be in the least bit tasty was noticed immediately. Vomiting was induced and he promptly brought up the tablets and remains of the packet. Activated charcoal was also administered.
We are delighted to report that he is back to his normal self and suffered no ill-effects.